Article Overview
What is an Epidural Hematoma (EDH)?
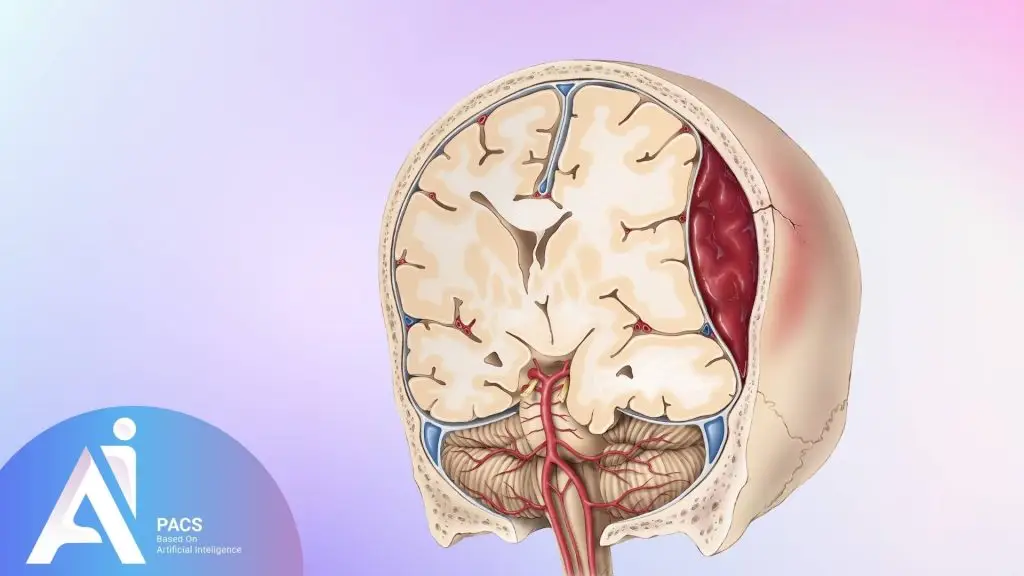
Epidural Hematoma (EDH) is a severe medical condition involving blood accumulation between the dura mater (the outer protective layer of the brain) and the skull. This condition often results from trauma to the head, which leads to the rupture of blood vessels, typically arteries. EDH can cause pressure to build up within the skull, leading to compression of brain tissue and, if untreated, potentially life-threatening complications. Understanding the causes, symptoms, and management of EDH is critical for rapid intervention.
Causes and Risk Factors: How Does EDH Occur?
EDH is most frequently linked to head injuries from high-impact incidents, such as motor vehicle accidents or falls. Athletes participating in contact sports like football or boxing are at elevated risk. Skull fractures, especially in the temporal region, increase the likelihood of EDH by damaging nearby blood vessels. Risk factors include anticoagulant use, which can exacerbate bleeding, and conditions that cause frailty of blood vessels, such as certain genetic disorders. Children are also particularly vulnerable due to their thinner skulls.
Signs and Symptoms of Epidural Hematoma
Early Warning Signs to Watch For
One of the most characteristic signs of EDH is the “lucid interval.” After the initial head injury, a person may seem alert and conscious, only to deteriorate rapidly as blood accumulates. Symptoms can develop within minutes or hours. Early signs include headache, dizziness, and nausea, often accompanied by confusion or disorientation. Sometimes, a patient may also experience a brief loss of consciousness, followed by an apparent recovery, only to lose consciousness again as the condition worsens.
Causes and Risk Factors: How Does EDH Occur?
As EDH progresses, more severe symptoms emerge, signaling increasing pressure on the brain. These include weakness or paralysis on one side of the body, dilated pupils, and seizures. As brain tissue is compressed, respiratory and heart rates can become irregular, potentially leading to coma or death. Severe headache, vomiting, and difficulty speaking are red flags that demand immediate medical evaluation.
The Role of Brain CT Scan in Diagnosing EDH
Why Brain CT Scan is the Gold Standard for EDH Detection
A Brain CT (Computed Tomography) scan is the most effective imaging tool for diagnosing EDH. It provides rapid, detailed cross-sectional images of the brain, allowing clinicians to see the location and size of the hematoma. Given the urgency of EDH, the ability to obtain real-time results makes CT scans invaluable. These scans offer high-resolution views of the skull and brain, helping detect skull fractures and any displacement of brain structures.
Causes and Risk Factors: How Does EDH Occur?
On a CT scan, EDH typically appears as a biconvex (lens-shaped) mass confined to a small brain area due to its separation by sutures. Hematoma often has well-defined edges, unlike other types of bleeding, which may spread more diffusely. The scan may also reveal midline shifts, where the brain is pushed to one side by the pressure of the hematoma. Early detection of these indicators is critical to determining the next steps in treatment.
Understanding the Severity of EDH
Classifying Epidural Hematoma: Mild, Moderate, and Severe Cases
Epidural hematomas can be classified based on their size, the degree of midline shift, and the patient’s neurological status. Mild cases may present with small hematomas and minimal symptoms, requiring observation.
Moderate instances in which the hematoma is more significant or causes neurological impairment often to necessitate more aggressive treatment. Severe
cases involving significant brain compression require emergency surgery to prevent permanent damage or death.
The Importance of Timely Diagnosis in Managing EDH
Prompt diagnosis and intervention are paramount. EDH can progress rapidly, and a delay in treatment can lead to irreversible brain damage or death. The time between injury and intervention, known as the “golden hour,” is critical. During this time, swift diagnosis via CT scan and immediate treatment can drastically improve outcomes.
Epidural vs. Subdural Hematoma: Key Differences
Classifying Epidural Hematoma: Mild, Moderate, and Severe Cases
While both EDH and subdural hematoma (SDH) involve bleeding in the brain, they differ in their location and mechanism. EDH occurs between
the dura and the skull, while SDH occurs between the dura and the brain. SDH
often involves slower venous bleeding, while EDH usually involves rapid
arterial bleeding, making EDH more acute. SDH tends to be more diffuse, whereas
EDH is more localized.
Other Brain Injuries to Consider When Reviewing a CT scan
When reviewing a brain CT scan, it’s essential to differentiate EDH from other traumatic injuries, such as cerebral contusions, intraparenchymal hemorrhages, and diffuse axonal injury. Each condition has distinct radiological features; misdiagnosis can lead to improper treatment. Understanding these nuances is essential for accurate diagnosis.
Treatment Options for Epidural Hematoma
Surgical Interventions: Craniotomy and Other Procedures
For many patients with EDH, surgery is the only viable treatment. A craniotomy, in which part of the skull is removed to access and
drain the hematoma, is the most common procedure. In some cases, burr hole
surgery, a less invasive procedure, may be performed to drain more minor
hematomas. Surgery aims to relieve pressure on the brain and prevent further
damage. After surgery, patients are monitored in intensive care to ensure brain
swelling does not occur.
Non-Surgical Management: When is it Appropriate?
In select cases where the hematoma is small and the patient is neurologically stable, conservative management may be considered. This typically involves close monitoring in a hospital setting with frequent CT scans to ensure the hematoma does not enlarge. Patients may also be prescribed medications to reduce intracranial pressure. Non-surgical approaches are rare but can be appropriate in mild cases.
Potential Complications of EDH
What Can Go Wrong: Complications to Be Aware Of
Complications from EDH can arise even after treatment. Seizures are a common issue, as the brain tissue may become irritated by the
presence of blood. Infections, particularly following surgery, are another
risk. Brain swelling and herniation, where brain tissue is displaced due to
increased pressure, are life-threatening complications that require immediate
intervention.
How to Minimize Risks and Improve Outcomes
Close monitoring is essential to reduce the risk of complications. Timely follow-up CT scans can help ensure the hematoma does not reoccur or expand. Proper wound care after surgery minimizes the risk of infection. Long-term management with anticonvulsant medications may be necessary for patients prone to seizures.
Prevention of Epidural Hematoma
Practical Steps to Prevent Head Trauma
Preventing head trauma is the best way to avoid EDH. Protective gear like helmets is crucial for at-risk individuals, such as athletes. In motor vehicles, seatbelt use and adherence to speed limits significantly reduce the risk of head injury. For older adults, fall prevention measures, such as using handrails and ensuring proper lighting, can reduce the
likelihood of trauma.
Protective Measures for High-Risk Individuals
People on anticoagulant medications or those with a history of head trauma should be particularly vigilant. These individuals should avoid activities that carry a high risk of falls or impacts. Regular check-ups with healthcare providers to review medication usage and assess fall risk can prevent injuries that could lead to EDH.
Conclusion
Recap: Why Fast Detection and Treatment of EDH is Crucial
Epidural Hematoma is a medical emergency that requires immediate attention. With prompt diagnosis and intervention, the outcomes can
be positive, but any delay in treatment can lead to irreversible damage. Brain
CT scans are indispensable in the swift detection of EDH, allowing healthcare
providers to act quickly and efficiently.
Final Thoughts: How a Brain CT Scan Saves Lives
A Brain CT scan can be the difference between life and death when it comes to EDH. By rapidly identifying the presence and extent of the hematoma, it allows for immediate medical intervention. With the proper treatment at the right time, patients with EDH can recover fully and avoid potentially devastating outcomes.