Mammography as a screening tool for breast health
Mammography plays a crucial role in the early detection of breast abnormalities, helping to identify potential issues before symptoms appear.
Calcifications as one of the findings on mammograms
One common mammogram finding is calcifications, tiny calcium deposits in the breast tissue visible as small white spots.
What calcification mean in mammography results
It is important to understand the meaning of calcifications in mammography results, as they can range from benign to potentially suspicious and require further evaluation.
Learn more about the BIRADS classification system and how it helps with early breast cancer detection.
What Are Calcifications?
Calcifications are tiny deposits of calcium that form in the breast tissue. They appear as white spots or flecks on a mammogram and are a common finding, especially in women over 50. While calcifications are not cancerous, their pattern, size, and distribution can provide important clues about underlying breast conditions. There are two main types:
Macrocalcifications: Large, coarse deposits usually benign and unrelated to cancer.
Microcalcifications: Smaller, clustered deposits that may sometimes indicate early signs of breast cancer, especially if their appearance is irregular or concentrated in one area.
Differentiating between microcalcifications and macrocalcifications:
These two types have differences in size, appearance, etc., which we will discuss further.
Macrocalcifications
Size: Larger, coarse calcium deposits.
Appearance: Scattered or spread out in the breast tissue, typically easy to identify.
Common Causes: Normal aging, previous breast injury, inflammation, or benign conditions like cysts.
Significance: Almost always benign and not associated with cancer, requiring no further testing or treatment.
Microcalcifications
Size: Smaller, fine calcium deposits.
Appearance: Can appear as clusters or irregular patterns.
Common Causes: These may be associated with benign conditions or indicate more concerning changes, such as Ductal Carcinoma In Situ (DCIS) or early-stage breast cancer.
Significance: This requires closer evaluation, and if the pattern is suspicious, further diagnostic steps, like a biopsy, may be recommended to rule out cancer.
Causes of Calcifications
Calcifications can have benign or malignant causes.
Benign causes
Aging: Natural changes in breast tissue over time.
Previous breast injuries: Trauma or surgery can lead to calcium deposits as the tissue heals.
Infections: Conditions like mastitis can result in calcifications.
Benign breast conditions like fibroadenoma or cysts: Non-cancerous growths like fibroadenomas or cysts often lead to calcifications.
Radiation Therapy: Previous radiation treatment can leave calcium deposits in breast tissue.
Potentially suspicious causes
Ductal carcinoma in situ (DCIS): A non-invasive form of breast cancer often associated with clustered microcalcifications.
Invasive Breast Cancer: Some patterns of calcifications may suggest early signs of invasive cancer.
Atypical Hyperplasia: Abnormal cell growth in breast ducts or lobules may lead to suspicious calcifications.
How Are Calcifications Detected?
Calcifications can be detected in mammography diagnostic tests that should be performed regularly.
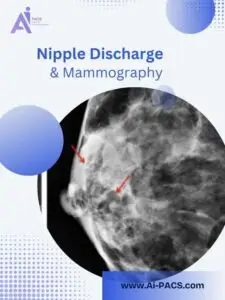
Role of mammograms in detecting calcifications
Mammograms are specialized X-ray images of the breast that play a crucial role in detecting calcifications. During the procedure, the breast is compressed, and X-rays are taken, highlighting areas of dense tissue and revealing any calcium deposits. Calcifications appear as small white spots or dots on the mammogram, and their size, shape, and distribution can provide important information about their nature.
Importance of radiologist expertise in interpreting calcification patterns
Interpreting calcifications requires specialized training and experience. Radiologists analyze the mammogram for specific patterns of calcifications to determine their significance:
- Benign vs. Suspicious Patterns: Radiologists look for characteristics such as clustering, shape, and size to differentiate between benign macrocalcifications and potentially concerning microcalcifications.
- Contextual Analysis: To provide a comprehensive assessment, the doctor considers the patient’s medical history, risk factors, and previous imaging results.
- Follow-up Recommendations: Based on their interpretation, radiologists may recommend additional imaging, such as diagnostic mammograms or ultrasounds, or further evaluation through biopsy if suspicious calcifications are identified.
This expertise is essential for accurate diagnosis and appropriate management of breast health.
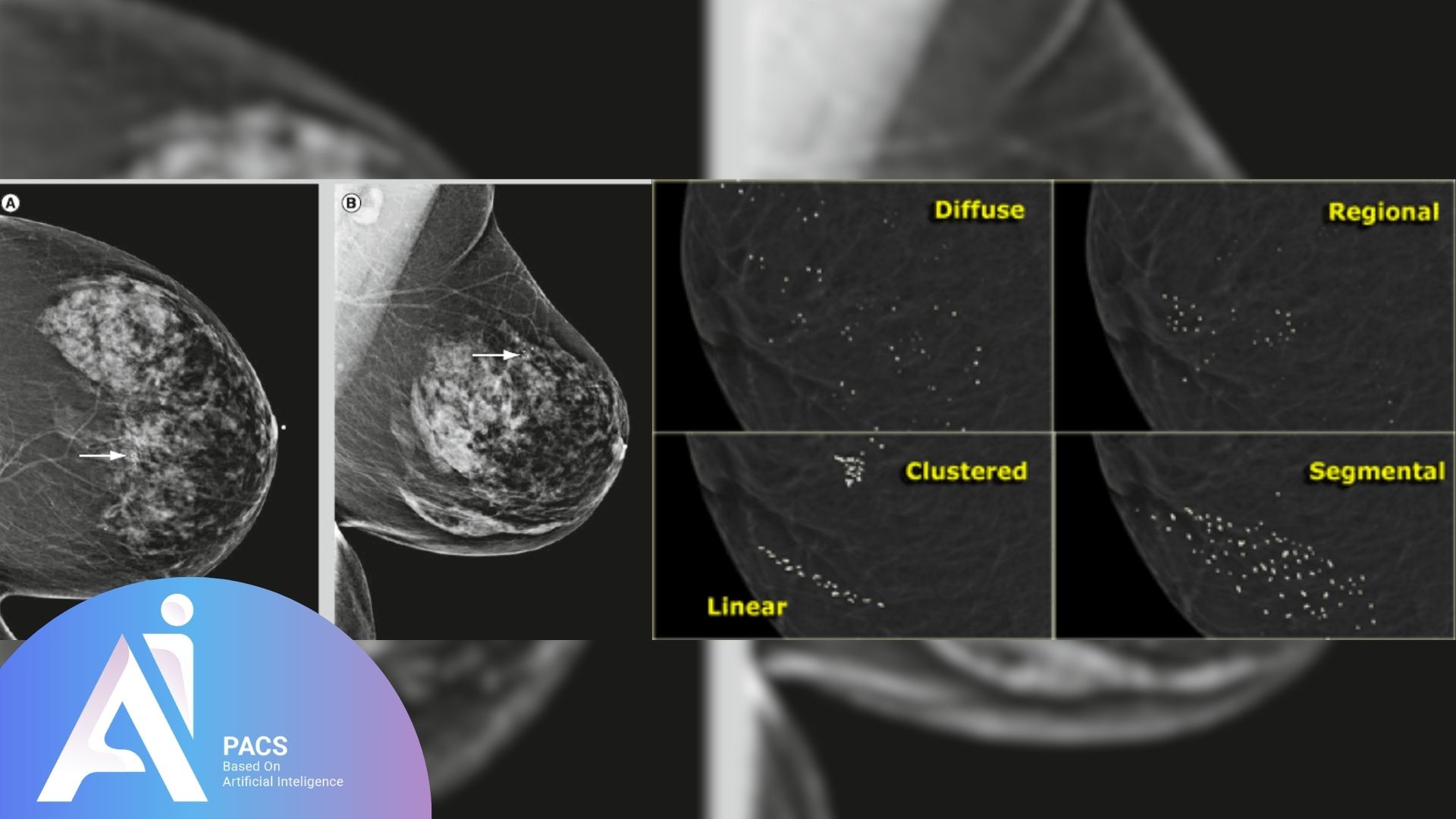
Calcification Patterns and Their Significance
Benign calcification patterns
Scattered Macrocalcifications: Large, coarse calcium deposits spread randomly throughout the breast tissue. These are common in aging and benign conditions and require no further action.
Popcorn Calcifications: Large, irregularly shaped calcifications that develop in benign growths like fibroadenomas as they age. They have a distinctive “popcorn” appearance and are unrelated to cancer.
Vascular Calcifications: Calcifications that form along the blood vessels within the breast. These are benign and often seen in older women, especially those with diabetes or heart disease.
Ring-Like (Eggshell) Calcifications: Thin, circular deposits surrounding cysts or benign masses, usually indicating non-cancerous conditions.
Suspicious calcification patterns
Clustered Microcalcifications: Small calcium deposits that appear closely grouped. These patterns are concerning because they can suggest the presence of abnormal cells or early-stage breast cancer, such as Ductal Carcinoma In Situ (DCIS).
Linear or Branching Calcifications: Microcalcifications arranged in a line or branching pattern may suggest the presence of abnormal cell growth within the milk ducts, potentially indicating a malignancy.
Heterogeneous or Irregularly Shaped Calcifications: These calcifications vary in size and shape and may be associated with more concerning underlying processes, warranting further investigation.
Suspicious patterns often require additional imaging, closer monitoring, or a biopsy to determine whether they are associated with cancerous changes.
What Happens if Calcifications Are Detected?
When calcifications are found during a routine mammogram, the next steps depend on their characteristics. No immediate action may be needed if they appear benign, but suspicious calcifications often require further evaluation. Below are more detailed explanations of the diagnostic steps that may follow the detection of calcifications.
Additional mammogram views (magnified images for closer evaluation)
Purpose: To get a more detailed view of the calcifications. Radiologists may request additional views if initial mammogram images show microcalcifications that appear clustered or have irregular shapes.
Procedure:
- A diagnostic mammogram is performed, which includes taking magnified images of the specific area where the calcifications are seen.
- These zoomed-in images allow radiologists to closely examine the calcifications’ size, shape, and distribution.
Outcome: This helps determine whether the calcifications are benign or suspicious, which guides the need for further testing or a biopsy.
Breast ultrasound or MRI
Breast Ultrasound:
- Purpose: Often used to complement mammography, particularly in women with dense breast tissue. Ultrasound may be ordered if calcifications are found, though it is more commonly used for evaluating lumps or masses rather than calcifications themselves.
- Procedure: The ultrasound uses sound waves to create detailed images of breast tissue and can help detect abnormalities that are harder to see on a mammogram.
- Outcome: Can provide more information about whether there is an associated mass near the calcifications. If no mass is found, and the calcifications appear benign, further intervention may not be needed.
Breast MRI:
- Purpose: Sometimes used to gather more detailed images, especially if mammograms and ultrasounds are inconclusive or if the calcifications are highly suspicious.
- Procedure: A breast MRI uses magnetic fields and contrast dye to create detailed images of breast tissue, helping to detect abnormalities that may be hidden on mammograms.
- Outcome: MRI can provide more insight into whether the calcifications are associated with a malignancy, which is particularly useful in high-risk women or when early breast cancer is suspected.
Biopsy (if calcifications appear suspicious for cancer)
Purpose: If calcifications show suspicious patterns—such as tight clusters, irregular shapes, or linear arrangements—further testing via a biopsy is often recommended to determine if they are cancerous or benign.
Types of Biopsies:
- Stereotactic Needle Biopsy:
- This is a common method used to evaluate suspicious calcifications. The biopsy is guided by mammography, and a needle removes small tissue samples from the area where the calcifications are located.
- Procedure: The patient lies face down, and the breast is positioned and compressed, similar to a mammogram. The radiologist uses X-rays to precisely g
uide the needle to the area of concern and extracts tissue samples for analysis.
- Surgical Biopsy:
- In some cases, a surgical biopsy (excisional biopsy) may be needed if the area is difficult to access with a needle. This procedure removes the entire area of suspicious calcifications for a more thorough examination.
Outcome: A pathologist examines the tissue under a microscope to determine whether cancerous or pre-cancerous cells are present. If the results are benign, regular follow-ups may be suggested. If cancer is detected, appropriate treatment options are discussed.
Each step aims to provide a clearer picture of the nature of the calcifications, ensuring that any necessary follow-up or treatment is timely and appropriate.
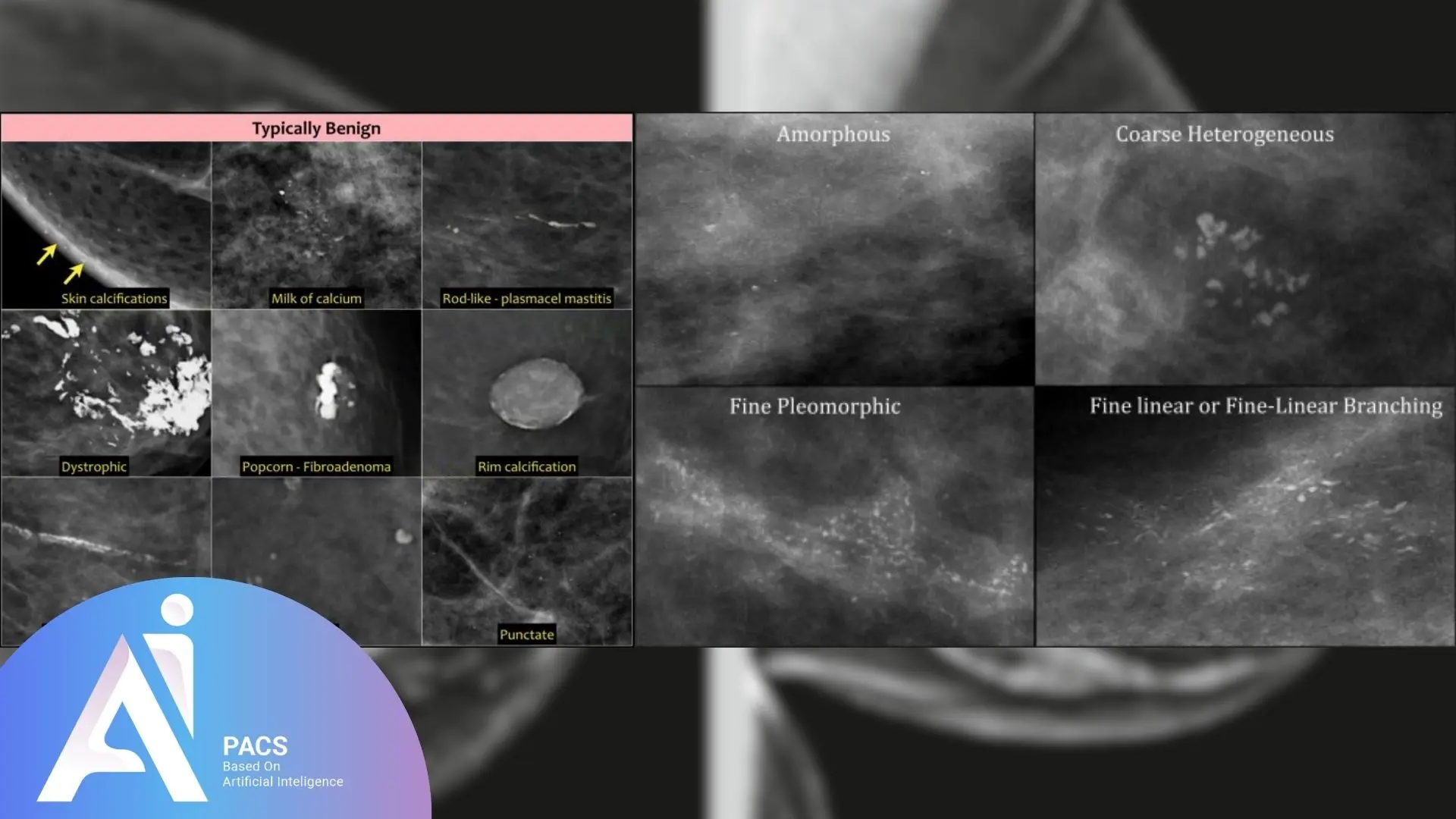
Benign vs. Suspicious Calcifications
Benign Calcifications
Characteristics:
- Larger, coarse deposits (macrocalcifications).
- Scattered throughout the breast tissue.
- Regular shapes, often round or oval.
- Seen in normal aging, previous breast injuries, or benign conditions like fibroadenomas and cysts.
Examples:
- Popcorn-like calcifications (from benign fibroadenomas).
- Vascular calcifications (along blood vessels).
Risk:
- Typically harmless and not associated with cancer.
- No further testing is usually required, but regular monitoring may be recommended.
Suspicious Calcifications
Characteristics:
- Smaller, fine deposits (microcalcifications).
- Clustered in tight groups or linear/branching patterns.
- Irregular or varying shapes and sizes.
- May indicate abnormal cell growth, such as Ductal Carcinoma In Situ (DCIS) or early-stage invasive cancer.
Examples:
- Clustered microcalcifications.
- Linear or branching calcifications in the milk ducts.
Risk:
- These patterns may suggest the presence of cancer or pre-cancerous changes.
- Often require further diagnostic tests, such as additional imaging or a biopsy, to rule out malignancy.
Understanding the differences between benign and suspicious calcifications is critical in determining whether further action is needed.
How Often Should You Be Screened?
The frequency of mammograms depends on factors like age, personal risk, and family history. General guidelines include:
Women Aged 40-49: Individualized decision-making is recommended. Depending on personal risk factors, some may begin screening every 1-2 years.
Women Aged 50-74: It is generally advised to have a mammogram every 1-2 years. Regular screenings in this age group help detect breast changes early, improving the chances of successful treatment.
High-Risk Individuals: Women with a family history of breast cancer, genetic predispositions (e.g., BRCA mutations), or other risk factors may need to start screening earlier and may require more frequent tests or additional imaging, like MRI.
Consulting with a healthcare provider is essential to determine the best screening schedule based on personal risk factors.
Conclusion
Understanding calcifications in mammography is critical to making informed decisions about breast health. While most calcifications are benign and pose no risk, some patterns may indicate the need for further evaluation to rule out or confirm more severe conditions like early-stage breast cancer. Regular mammograms, combined with the expertise of your healthcare provider, help ensure that any concerning findings are identified and addressed promptly. Staying informed and proactive in following up on your mammogram results is essential to maintaining breast health and ensuring early detection when necessary. Concerned about your mammogram results? Get an expert second opinion. Upload your report now for a comprehensive analysis.