Introduction to PCOS and Its Impact on Health
Polycystic Ovary Syndrome (PCOS) is a common hormonal and metabolic disorder that affects women of reproductive age, impacting up to 10% of women worldwide. PCOS is marked by an imbalance in reproductive hormones, often leading to irregular menstrual cycles, excess androgen levels, and the development of small cysts on the ovaries. Beyond reproductive health, PCOS can also affect metabolic health, contributing to insulin resistance, weight gain, and an increased risk for type 2 diabetes and cardiovascular diseases.
Accurate diagnosis of PCOS is crucial, as early identification allows for better management of symptoms and reduces the risk of long-term health complications. Diagnostic tools like ultrasound and clinical and biochemical evaluation help ensure a comprehensive approach to diagnosing and treating PCOS, improving health outcomes and quality of life for those affected.
Diagnostic Criteria for PCOS
The diagnosis of Polycystic Ovary Syndrome (PCOS) relies on a combination of clinical signs, laboratory findings, and, often, ultrasound imaging. Medical professionals typically refer to the Rotterdam criteria, which require at least two of the following three conditions to be present for a PCOS diagnosis: irregular or absent ovulation (leading to menstrual irregularities), elevated androgen levels (or symptoms thereof), and polycystic ovarian morphology observed via ultrasound.
Role of Clinical Signs
Key clinical signs are often the first indicators of PCOS. Elevated androgen levels cause hirsutism (excess hair growth on the face, chest, and back), acne, and scalp hair thinning. Menstrual irregularities, including infrequent or absent periods, are also common, signaling potential issues with ovulation. Recognizing these clinical signs is essential, as they often prompt further investigation into possible PCOS.
Significance of Laboratory Findings
Laboratory tests are crucial in confirming elevated levels of androgens, such as testosterone, which are common in PCOS. Blood tests may also reveal other hormonal imbalances, like increased luteinizing hormone (LH) or insulin resistance, that contribute to the metabolic aspects of PCOS. These lab findings, in combination with clinical signs, create a clearer diagnostic picture and help rule out other conditions with similar symptoms, such as thyroid disorders or hyperprolactinemia.
Together, clinical signs and laboratory findings provide a comprehensive approach to diagnosing PCOS, supporting personalized management strategies to address both reproductive and metabolic concerns.
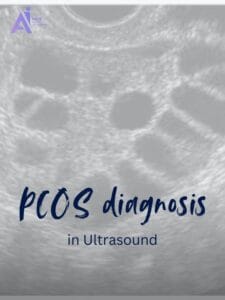
Role of Ultrasound in PCOS Diagnosis
Ultrasound imaging plays a crucial role in diagnosing Polycystic Ovary Syndrome (PCOS), offering a non-invasive way to observe ovarian morphology directly. When clinical symptoms and laboratory findings suggest possible PCOS, ultrasound is often used to confirm or support the diagnosis, as it provides real-time visualization of the ovaries.
Why Ultrasound is Used
Ultrasound is an essential diagnostic tool because it enables clear imaging of ovarian structure, helping to assess the number and appearance of follicles and overall ovarian size. This imaging is integral to meeting the Rotterdam criteria, which consider polycystic ovarian morphology (PCOM) one of the three main diagnostic markers for PCOS. Using ultrasound adds specificity to the diagnosis, particularly when clinical signs may be inconclusive, or hormone levels are borderline.
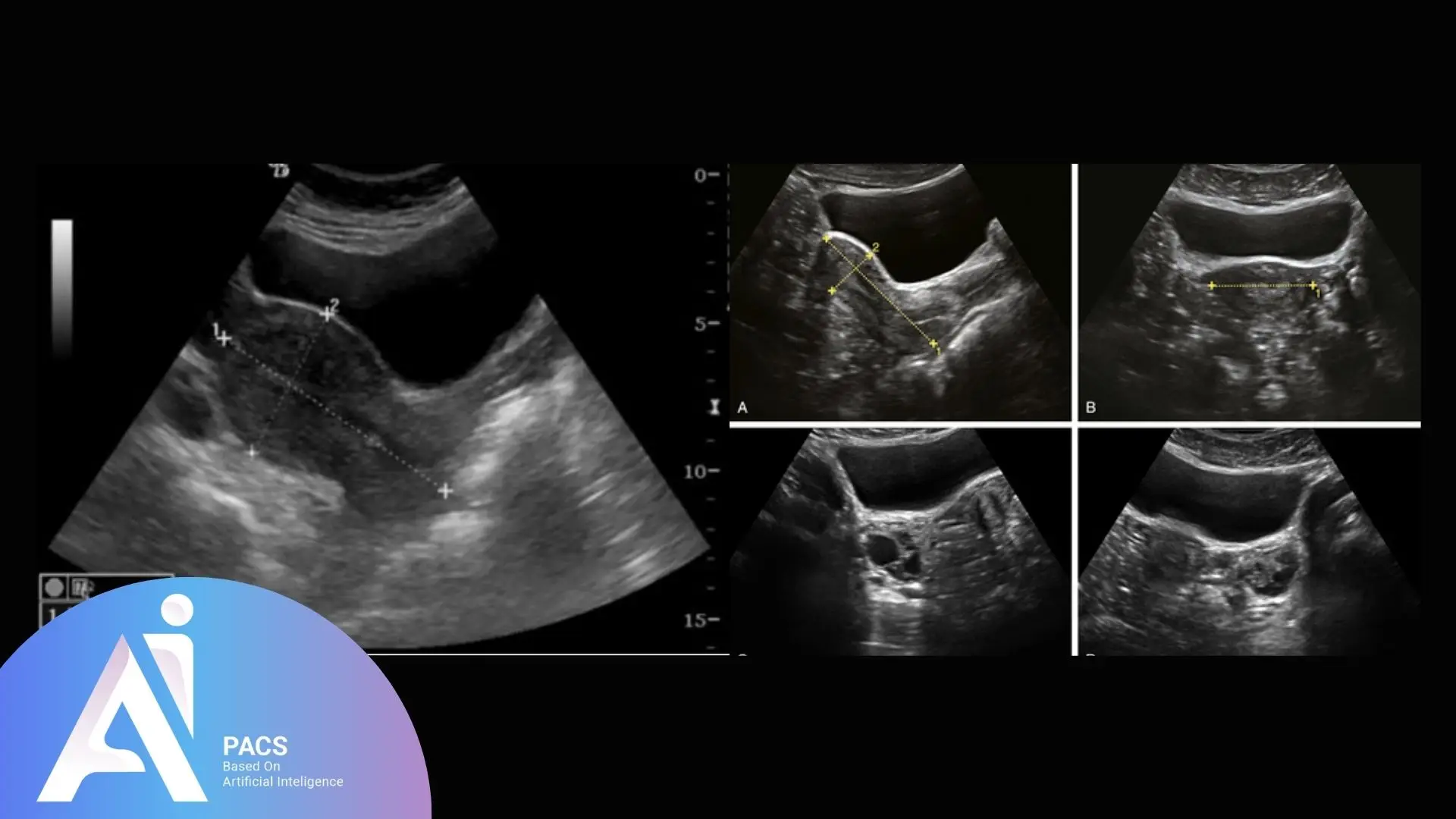
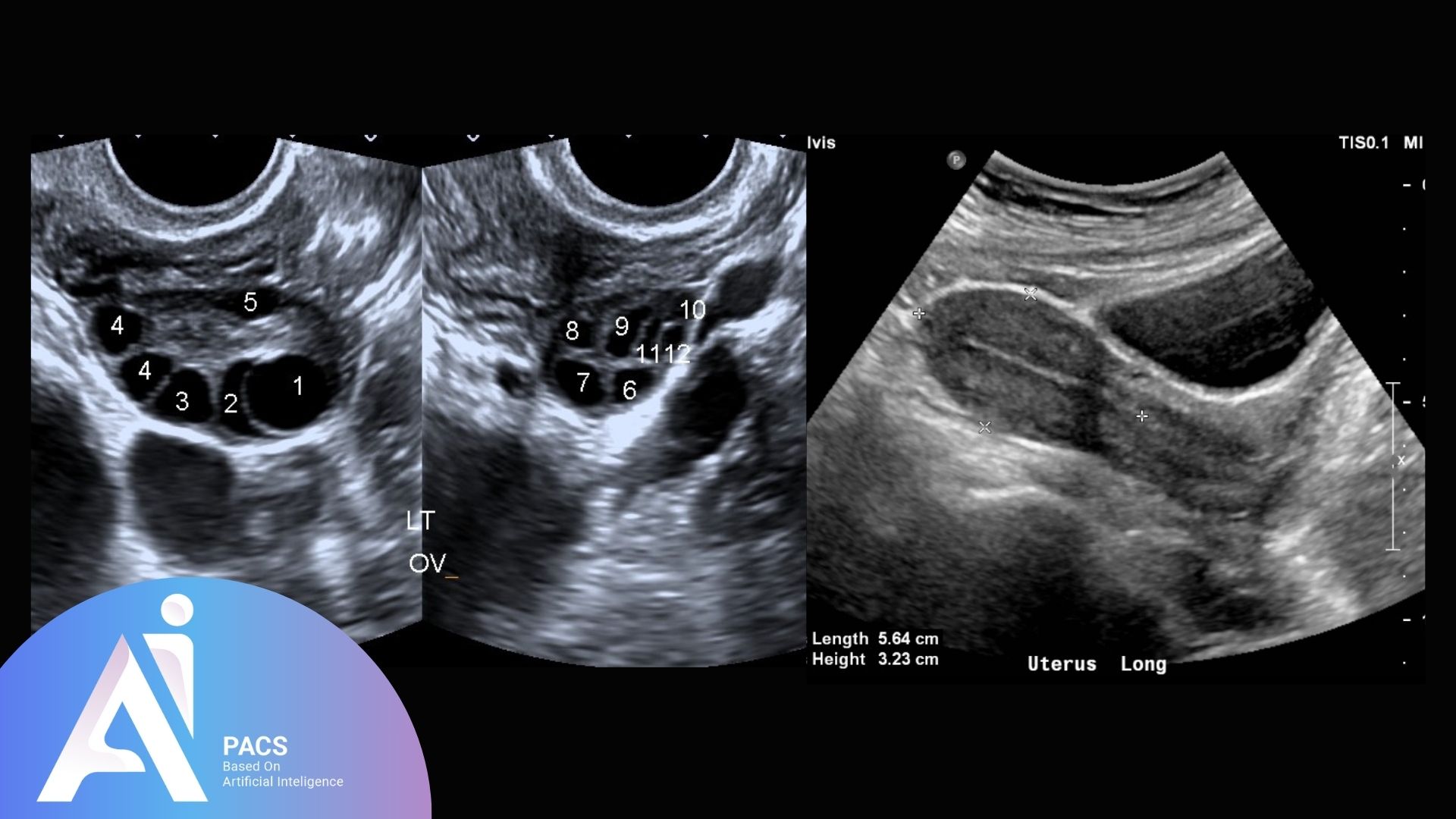
What Ultrasound Reveals About Ovarian Morphology
On ultrasound, ovaries affected by PCOS often display a distinctive appearance. Key indicators include an increased number of small, fluid-filled follicles (usually 12 or more per ovary) arranged in a “string of pearls” pattern along the periphery of the ovary. Additionally, affected ovaries tend to have a larger volume than normal. These morphological characteristics are specific to PCOS and aid clinicians distinguish it from other conditions that may affect the ovaries.
By using ultrasound to reveal these detailed aspects of ovarian structure, healthcare providers can make more accurate diagnoses and tailor treatment plans to the individual’s needs, improving the management of both reproductive and metabolic symptoms associated with PCOS.
Ultrasound Features of PCOS
Ultrasound imaging reveals specific features in the ovaries that are characteristic of Polycystic Ovarian Syndrome (PCOS). These features are essential for confirming a PCOS diagnosis when combined with clinical and hormonal indicators, as outlined by diagnostic criteria like the Rotterdam criteria. By closely examining ovarian volume, follicle count, and distribution, ultrasound allows practitioners to distinguish between normal and polycystic ovarian morphology.
Key Features: Ovarian Volume and Follicle Count
The two primary ultrasound indicators of PCOS are ovarian volume and follicle count. In PCOS, the ovaries are often enlarged, with a volume exceeding ten cm³. Additionally, affected ovaries typically contain more small follicles; generally more than 12 per ovary, each measuring 2–9 mm in diameter. These follicles are often arranged peripherally in a “string of pearls” pattern. This high follicle count and larger ovarian volume are strong indicators of PCOS and are used as critical diagnostic markers.
Differentiating Between Normal and Polycystic Ovaries
Normal ovaries contain fewer follicles (usually less than 12), often distributed more evenly throughout the ovary rather than clustered along the outer edge. Normal ovarian volume is also smaller than in PCOS, typically less than ten cm³. The differences in follicle distribution, size, and ovarian volume help distinguish polycystic ovaries from healthy ovaries and other abnormalities like simple ovarian cysts.
Visual Examples of PCOS and Non-PCOS Ovaries
On ultrasound images, polycystic ovaries present a distinct appearance. In PCOS, the high follicle count, peripheral arrangement of follicles, and larger ovarian size create a recognizable pattern. In contrast, non-PCOS ovaries appear less dense, with fewer more dispersed follicles and a smaller overall ovarian volume. These visual differences on ultrasound are instrumental in confirming a diagnosis of PCOS, allowing for more targeted and effective patient care.
Through these distinctive ultrasound features, clinicians can more accurately diagnose PCOS and implement individualized treatment plans that address reproductive and metabolic health concerns.
Challenges and Limitations in Ultrasound Diagnosis
While ultrasound is a valuable tool for diagnosing Polycystic Ovary Syndrome (PCOS), several challenges and limitations can affect its diagnostic accuracy. Understanding these factors is crucial for clinicians to interpret ultrasound results effectively and consider the need for additional diagnostic methods.
Factors Affecting Diagnostic Accuracy
Several factors can influence the accuracy of ultrasound findings in PCOS diagnosis:
- Age: The patient’s age can significantly affect ovarian morphology. In younger women, multiple small follicles may be more common and can sometimes be misinterpreted as polycystic ovaries. Conversely, older women may exhibit a natural decline in ovarian reserve, which can complicate the interpretation of ultrasound findings.
- Obesity: Obesity is prevalent among women with PCOS and can introduce additional variables in ultrasound imaging. Increased adipose tissue can obscure visualization of the ovaries, making it harder to assess their size and morphology accurately. Furthermore, obesity can lead to changes in hormone levels, potentially masking typical PCOS characteristics.
- Timing of the Examination: The menstrual cycle phase during which the ultrasound is performed can also impact the findings. For instance, an ultrasound during the follicular phase may yield different results than during the luteal phase, affecting follicle count and size.
Sensitivity and Specificity Limitations
Ultrasound also has inherent limitations regarding sensitivity and specificity in diagnosing PCOS:
- Sensitivity: The sensitivity of ultrasound in identifying PCOS can vary. While it effectively detects the characteristic features of polycystic ovaries, it may not capture all cases, particularly in early or mild forms of the syndrome. Some women with PCOS may present with normal ovarian morphology, leading to false negatives.
- Specificity: The specificity of ultrasound in diagnosing PCOS can be compromised due to the overlap of ultrasound features with other conditions. For example, multiple follicles can occur in conditions like functional ovarian cysts or during normal ovarian activity in younger women. This overlap can result in misdiagnosis or uncertainty in interpretation.
While ultrasound is essential in the diagnostic process for PCOS, its challenges and limitations necessitate a comprehensive approach. Clinicians should combine ultrasound findings with clinical evaluations and laboratory results to improve diagnostic accuracy and provide effective management strategies for women with PCOS.
Interpretation and Reporting
The interpretation and reporting of ultrasound findings in Polycystic Ovary Syndrome (PCOS) are critical components of the diagnostic process. Accurate interpretation not only aids in confirming the diagnosis but also informs treatment decisions and patient management strategies. To achieve this, clinicians must adhere to standardized protocols and clear communication practices.
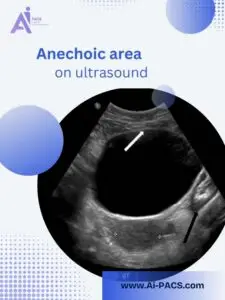
Understanding Ultrasound Findings
When interpreting ultrasound results, radiologists and clinicians look for specific morphological characteristics of the ovaries. Key features include:
- Ovarian Volume: Measurements exceeding ten cm³ may indicate PCOS.
- Follicle Count: An assessment of the number of follicles in each ovary, with more than 12 follicles measuring 2–9 mm typically suggestive of polycystic ovaries.
- Follicular Distribution: The presence of follicles arranged in a “string of pearls” pattern along the periphery of the ovaries is a classic sign of PCOS.
Understanding these features is essential for differentiating between normal and polycystic ovarian morphology and ruling out other ovarian disorders.
Importance of Standardized Reporting
Standardized reporting formats enhance the clarity and consistency of ultrasound findings. A structured report may include:
- Patient Information: Basic demographic and clinical history.
- Ultrasound Technique: Description of the imaging method used (e.g., transvaginal or transabdominal).
- Ovarian Measurements: Specific measurements of each ovary, including volume and follicle count.
- Descriptive Findings: Detailed observations regarding the appearance of the ovaries and any other relevant structures.
- Conclusions: A summary statement indicating whether the findings are consistent with PCOS or if further evaluation is needed.
Communication with Clinicians
Effective communication of ultrasound findings is vital for ensuring appropriate follow-up and management. Radiologists should provide clear, concise reports highlighting the key diagnostic features and any uncertainties or recommendations for further investigation. This collaboration between radiologists and referring clinicians is crucial for the timely and accurate diagnosis of PCOS.
Want to learn more about diagnostic imaging and understanding reports during pregnancy? Check out our guide on Understanding Your Second-Trimester Ultrasound Reports to decode key terms and what they mean for your health.
Conclusion
In summary, ultrasound plays a pivotal role in the diagnosis of Polycystic Ovary Syndrome (PCOS), providing essential insights into ovarian morphology that aid in confirming the condition. By evaluating key features such as ovarian volume and follicle count, healthcare providers can effectively differentiate between normal and polycystic ovaries. However, the interpretation and reporting of ultrasound findings come with challenges, including variability due to factors like age, obesity, and the timing of examinations and limitations in sensitivity and specificity.
To achieve accurate diagnoses, it is crucial to integrate ultrasound results with clinical signs and laboratory findings while adhering to standardized reporting practices. Clear communication between radiologists and referring clinicians enhances patient management and ensures that individuals with PCOS receive appropriate care. As advancements in ultrasound technology and imaging techniques continue to evolve, they hold the potential to further improve the diagnostic accuracy and management strategies for PCOS, ultimately contributing to better health outcomes for those affected by this complex disorder.
Ready to take control of your health? Consult with our expert radiologists today to get a second opinion on your PCOS-related ultrasound reports.