What Are Hyperechoic Lesions and How Do They Appear on Ultrasound?
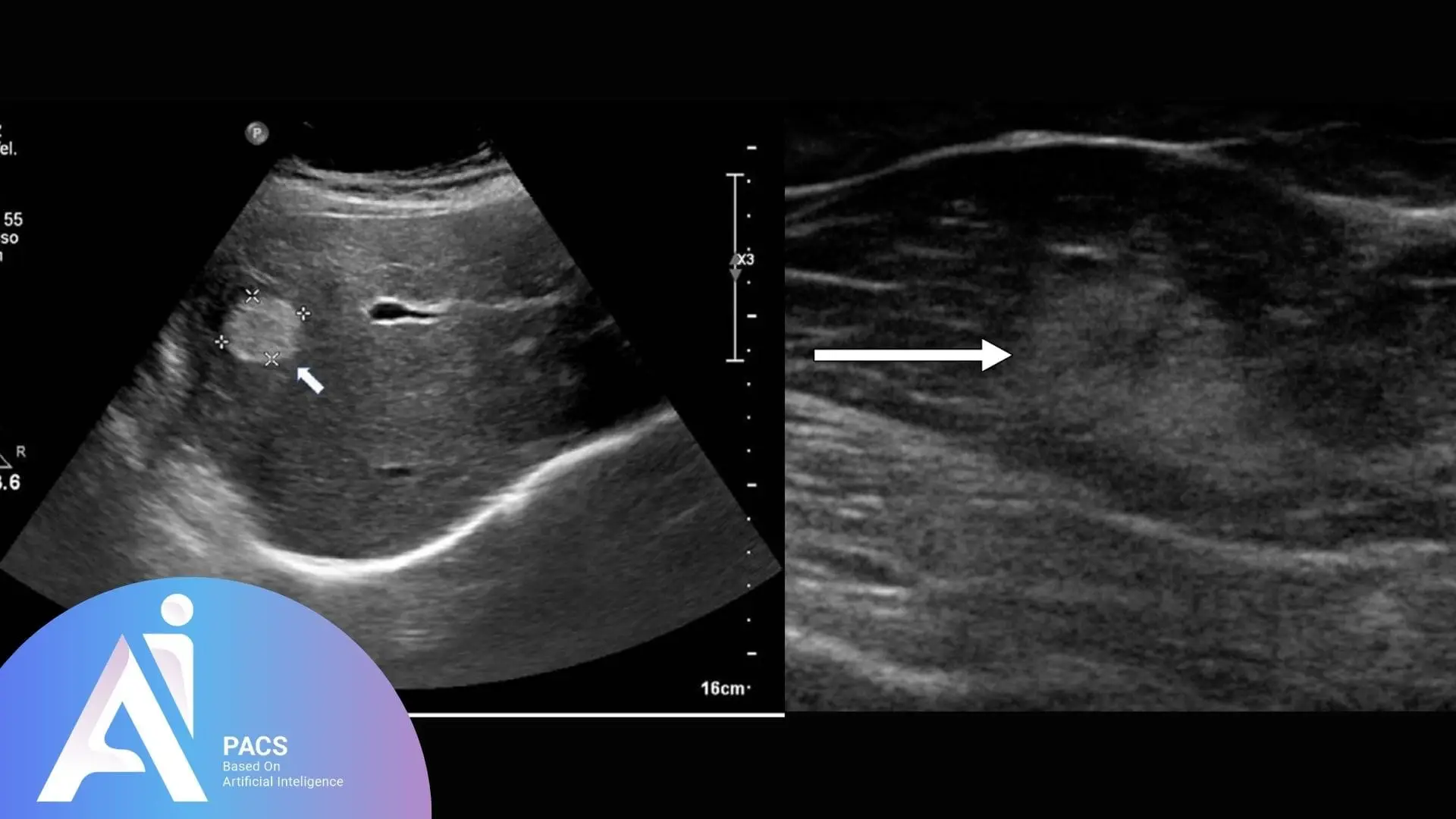
Hyperechoic lesions are regions in an ultrasound image that appear brighter than surrounding tissues. This increased brightness is due to the tissue’s higher reflectivity, as it bounces more sound waves to the ultrasound transducer. These lesions can indicate various conditions, ranging from benign tissue changes to more severe abnormalities. Recognizing their characteristics is essential for accurate diagnosis and clinical decision-making.
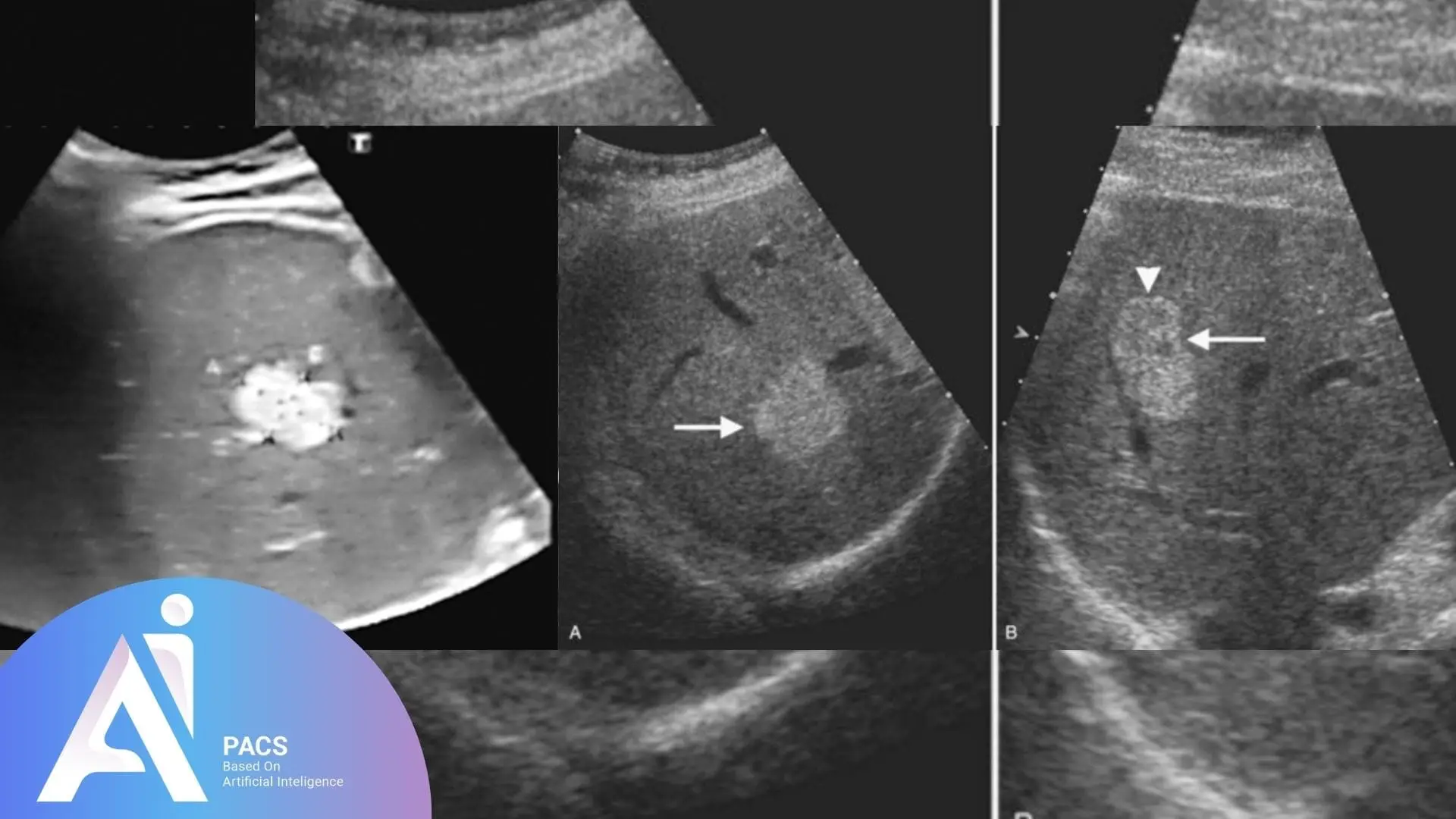
On an ultrasound scan, hyperechoic lesions are characterized by their bright, white appearance, contrasting with the darker shades of surrounding tissues. This brightness results from the lesion’s high density or specific composition, such as fat, calcifications, or fibrosis, which reflects sound waves more effectively. Factors like lesion size, shape, borders, and location are critical in determining the potential underlying cause. Advanced ultrasound techniques, such as Doppler or contrast-enhanced ultrasound, can further enhance the visualization and interpretation of these lesions.
👉 Upload your report now and get an expert review from AI-PACS online radiology report services.
What Causes Hyperechoic Lesions?
Hyperechoic lesions result from tissues or materials within the body that reflect ultrasound waves more strongly than their surroundings. These bright areas can occur in various organs and structures, each potentially indicating a range of underlying conditions. Understanding their causes helps differentiate between benign and pathological findings, aiding in accurate diagnosis and treatment planning.
Types of tissues or materials that cause hyperechogenicity
The composition of the tissue or material influences the appearance of hyperechoic lesions. Common contributors to hyperechogenicity include:
Fat: Fatty tissues naturally have high echogenicity, commonly seen in specific organs like the liver and kidneys.
Calcifications: Mineral deposits within tissues, such as calcium, strongly reflect sound waves and appear as distinct bright spots.
Fibrosis: Dense fibrous tissues, often due to scarring or chronic inflammation, also exhibit hyperechoic characteristics.
Air or Gas: Though not tissue, trapped air or gas bubbles can reflect sound waves and contribute to hyperechogenicity, particularly in the gastrointestinal system.
Common benign causes
Several benign conditions can lead to hyperechoic lesions, including:
- Lipomas: Fat-based tumors are usually harmless and often seen in subcutaneous or deeper tissues.
- Simple Calcifications: These are found in areas like the breast or liver and are generally related to aging or chronic inflammation.
- Fibrotic Changes: Scarring from injury or surgery may result in hyperechoic patterns, which are stable and non-progressive over time.
- Benign Cysts with Wall Calcifications: Occasionally, simple cysts develop calcified walls, appearing hyperechoic without significant clinical concern.
Pathological causes
Pathological conditions causing hyperechoic lesions require closer investigation, as they may indicate serious health concerns:
- Tumors: Certain solid tumors may present as hyperechoic lesions, particularly those with calcifications or fibrotic components. Examples include hepatocellular carcinoma or thyroid adenomas.
- Infections: Abscesses or granulomas may contain components like fibrosis or calcifications, causing bright echoes on ultrasound.
- Chronic Inflammatory Conditions: Diseases like cirrhosis or chronic pancreatitis can result in areas of hyperechogenicity due to fibrosis.
- Post-traumatic or Post-Surgical Scar Tissue: Abnormal healing or chronic scarring in tissues may lead to hyperechoic appearances.
Differentiating between benign and pathological causes requires careful interpretation of the lesion’s characteristics and clinical context, and often, further diagnostic tests, such as biopsy or advanced imaging.
Diagnostic Contexts of Hyperechoic Lesions
Hyperechoic lesions can appear in various medical imaging contexts, each offering valuable diagnostic insights into the health of specific organs or systems. Their appearance, location, and associated characteristics are interpreted differently depending on the type of ultrasound being performed.
Interpretation in abdominal ultrasound
In abdominal ultrasounds, hyperechoic lesions are commonly observed in organs like the liver, kidneys, pancreas, and gallbladder. These bright areas can signify:
- Liver Lesions: Fatty infiltrations, hemangiomas (benign vascular growths), or calcifications from chronic infections or previous trauma.
- Kidney Findings: Hyperechoic lesions may indicate renal stones, cysts with calcified walls, or angiomyolipomas (benign tumors with fatty components).
- Gallbladder Abnormalities: Gallstones often appear as highly hyperechoic areas with posterior acoustic shadowing.
- Pancreatic Conditions: Chronic pancreatitis or calcifications in the pancreas may produce hyperechoic patterns.
The context of these findings, patient history, and additional imaging help determine whether the lesion is benign or requires further evaluation.
Findings in musculoskeletal ultrasound
Musculoskeletal ultrasound often identifies hyperechoic lesions in muscles, tendons, and joints. Common interpretations include:
- Calcifications: Tendon calcifications, often due to chronic inflammation or degenerative changes, are frequent findings.
- Foreign Bodies: Hyperechoic artifacts may result from embedded objects like glass or metal fragments.
- Fatty Degeneration: In muscles, hyperechoic areas can indicate fatty atrophy or scarring from old injuries.
- Fibrosis or Scar Tissue: Post-injury or post-surgical fibrosis within tendons or ligaments often appears brighter.
Musculoskeletal findings are assessed with clinical symptoms such as pain, swelling, or restricted mobility.
Hyperechoic lesions in breast imaging
In breast ultrasounds, hyperechoic lesions often require detailed evaluation due to their potential implications:
- Benign Findings: Fibroadenomas, lipomas, or areas of fat necrosis often show hyperechogenicity and well-defined borders.
- Malignant Indicators: Certain cancers, particularly those with calcifications, may appear hyperechoic. However, irregular borders, posterior shadowing, and associated hypoechoic areas often raise suspicion.
- Post-Treatment Changes: Scarring from surgeries or radiation therapy can result in stable hyperechoic regions over time.
Breast imaging findings often correlate with mammograms or biopsies to confirm the diagnosis.
Significance in gynecological ultrasound
In gynecological ultrasounds, hyperechoic lesions may be seen in the uterus, ovaries, or surrounding structures. Key interpretations include:
- Uterine Findings: Fibroids with calcifications or adenomyosis can present as hyperechoic areas in the uterine wall.
- Ovarian Lesions: Dermoid cysts (teratomas) often contain fat or calcified elements, producing bright echoes.
- Endometrial Calcifications: Chronic endometritis or post-procedural changes may cause calcified lesions in the endometrial lining.
- Pelvic Masses: Occasionally, malignant masses may exhibit hyperechoic components, especially if calcifications are present.
The significance of these findings is assessed in conjunction with patient symptoms, hormonal status, and the need for further testing, such as CT, MRI, or surgical intervention.
Differentiating Hyperechoic Lesions
Hyperechoic lesions can vary widely in significance, from harmless findings to indicators of severe conditions. Differentiating these lesions involves assessing their specific characteristics and using complementary diagnostic tools to ensure accurate interpretation.
Role of shape, size, and border characteristics
The shape, size, and border of a hyperechoic lesion provide vital clues about its nature:
- Shape: Round or oval lesions are often benign, while irregularly shaped lesions may suggest malignancy or complex pathology.
- Size: Small lesions are commonly incidental and harmless, but larger lesions warrant closer evaluation for underlying causes.
- Borders:
Smooth and Well-Defined: Often indicates benignity, such as lipomas or simple cysts.
Irregular or Spiculated: More likely to be associated with malignant or invasive processes.
Halo Sign: A surrounding hypoechoic area may indicate inflammation or malignancy.
Careful examination of these features helps radiologists provide a more definitive diagnosis.
Comparing with hypoechoic and anechoic lesions
Understanding the differences between hyperechoic, hypoechoic, and anechoic lesions is essential for accurate interpretation:
- Hyperechoic Lesions: Appear bright due to solid reflection of ultrasound waves, often indicating dense or calcified tissues.
- Hypoechoic Lesions Appear darker and usually represent fluid-filled structures, soft tissue masses, or malignancies with low echogenicity.
- Anechoic Lesions: Completely black areas that indicate fluid-filled spaces, such as cysts or blood vessels, due to the absence of echo reflections.
Differentiating these types helps clinicians correlate imaging findings with the underlying tissue composition and pathology.
Importance of additional imaging modalities (CT, MRI)
While ultrasound is an excellent initial imaging tool, additional modalities like CT and MRI are often necessary for more detailed evaluation:
- CT Scans: Provide high-resolution images of calcifications, vascularity, and detailed anatomical structures. They are particularly useful for detecting hyperechoic masses in the abdomen or chest.
- MRI: Offers superior contrast resolution for soft tissue evaluation. It can accurately differentiate between fat, fibrosis, and other components of hyperechoic lesions.
- Contrast-Enhanced Imaging: Using contrast agents in CT and MRI can help determine vascularity, helping to differentiate benign from malignant lesions.
These modalities complement ultrasound findings, helping to confirm or rule out specific diagnoses.
When to be concerned about hyperechoic lesions
Specific characteristics of hyperechoic lesions raise red flags and may require further investigation:
- Rapid Growth: Indicates possible malignancy or aggressive pathology.
- Irregular Borders or Spiculations: Suggest invasive or malignant processes.
- Associated Symptoms: Pain, swelling, or systemic signs like fever may indicate infection or malignancy.
- Location in High-Risk Areas: Lesions in organs with higher cancer prevalence, such as the liver or breast, warrant additional scrutiny.
- Mixed Echogenicity: Hyperechoic lesions with hypoechoic or anechoic components can indicate complex cysts or malignant tumors.
If any of these features are present, further evaluation with biopsy, advanced imaging, or consultation with a specialist is recommended to ensure timely and appropriate management.
Conditions requiring biopsy or further tests
Specific hyperechoic lesions necessitate a biopsy or additional diagnostic tests to rule out malignancy or confirm the nature of the lesion. Key indicators include irregular borders, rapid growth, or mixed echogenicity, which may point to invasive or malignant processes. Lesions associated with systemic symptoms such as unexplained weight loss, fever, or pain raise suspicion and warrant further investigation. For instance, hyperechoic lesions in high-risk organs like the liver, breast, or thyroid are often biopsied to exclude cancer or other severe conditions.
Advanced modalities such as contrast-enhanced ultrasound, CT, or MRI can help refine the diagnosis in cases where imaging findings are inconclusive. However, when imaging and clinical findings suggest a potentially significant underlying pathology, a biopsy provides a definitive tissue diagnosis. This step is particularly crucial for lesions that demonstrate vascularity or irregular patterns on imaging, as these are common in malignancies. Timely biopsies or further tests ensure early detection and proper management of severe conditions.
Conclusion
In conclusion, hyperechoic lesions in ultrasound imaging are significant findings that require careful interpretation to differentiate between benign and pathological causes. Advances in ultrasound technology, such as elastography, contrast-enhanced imaging, and AI integration, have greatly improved the accuracy of lesion detection and characterization. Understanding the clinical context, assessing the lesion’s features, and utilizing complementary diagnostic tools like CT, MRI, or biopsy are crucial to ensure accurate diagnosis and appropriate management. Early evaluation and intervention concerning hyperechoic lesions can lead to better outcomes and more effective treatment strategies.