Why Is Medical Imaging Needed for Brain Tumors?
Medical imaging is a vital tool in the diagnosis and treatment of brain tumors, providing a range of benefits that enable doctors to deliver the best possible care. Here’s why it’s so important:
1. Early Detection and Accurate Diagnosis
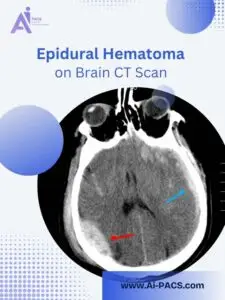
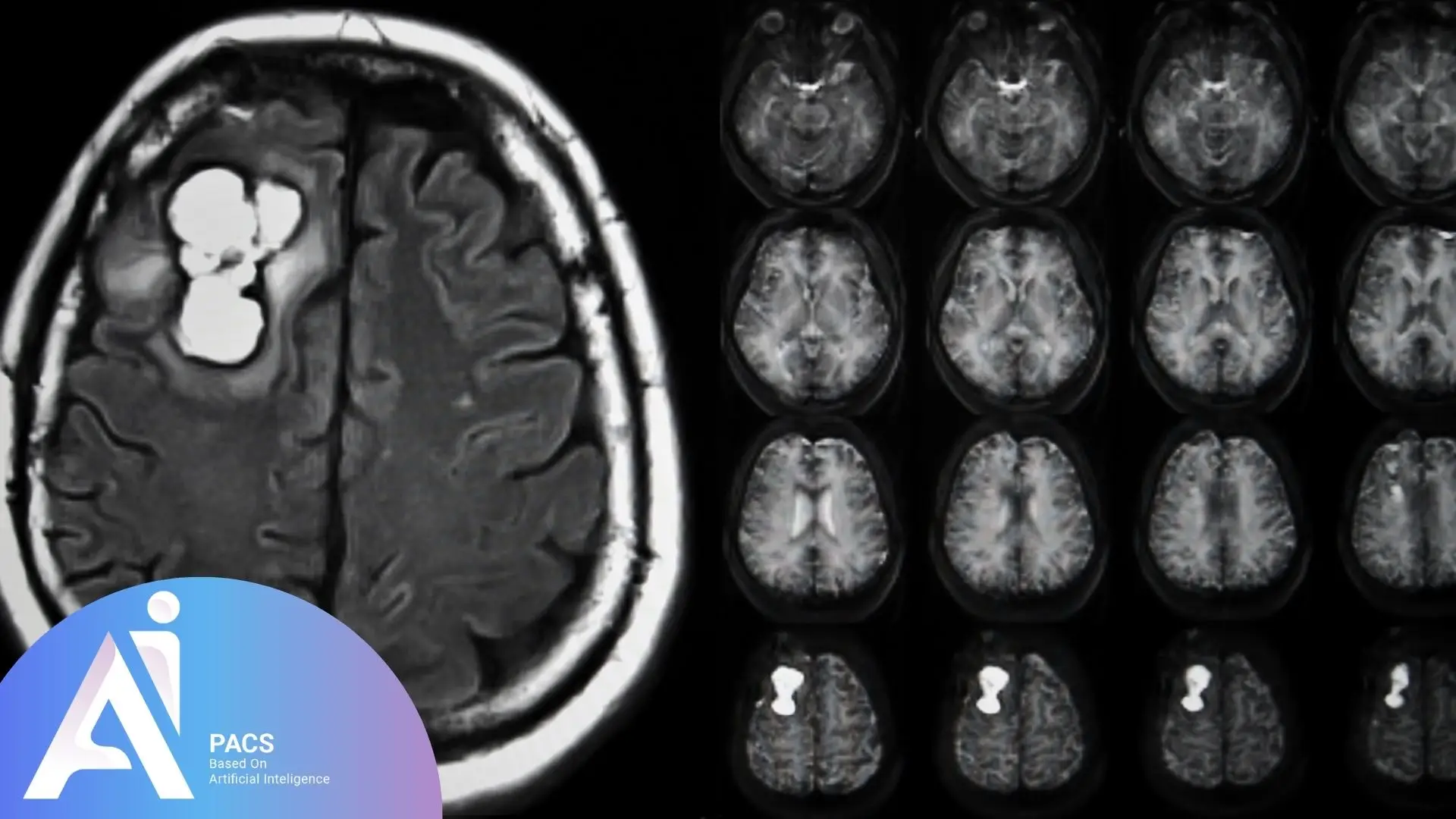
Brain tumors often present with vague symptoms like persistent headaches, seizures, or changes in memory and concentration. These symptoms can overlap with other neurological conditions such as multiple sclerosis (MS) or brain infections, making it hard to pinpoint the exact cause. Medical imaging, such as MRI (Magnetic Resonance Imaging) or CT scans, helps differentiate a brain tumor from other health issues by providing detailed, real-time images of the brain. For instance, an MRI can identify abnormal growths or swelling, which are indicative of a tumor, helping doctors make an early diagnosis before symptoms become more severe.
2. Tumor Localization and Characterization
Once a brain tumor is detected, the next step is to assess its size, location, and type. Is it a benign (non-cancerous) tumor, or is it malignant (cancerous)? Imaging techniques, particularly MRI and CT scans, provide high-resolution images that allow doctors to map the tumor’s position within the brain. For example, if a tumor is located near critical areas responsible for speech or motor skills, doctors can plan a more precise surgical approach to minimize damage. Furthermore, imaging helps to differentiate between various types of tumors, ensuring the proper treatment is prescribed.
3. Surgical Planning
Surgery is often the first line of treatment for brain tumors, especially if they are accessible. However, it’s a delicate procedure that requires precision to avoid damaging healthy brain tissue. Advanced imaging, such as functional MRI (fMRI), helps neurosurgeons plan the safest approach for tumor removal. The ability to visualize the tumor in 3D, along with its proximity to essential brain structures, significantly improves the surgeon’s ability to navigate the brain during the operation. For example, when dealing with tumors in speech-related areas, imaging can ensure surgeons avoid interfering with regions that control language.
In many cases, malignant primary brain tumors cannot be completely removed via surgery. This is why imaging is also used to guide radiation and chemotherapy treatments, ensuring these therapies target the tumor effectively while minimizing damage to surrounding tissues. (In my experience, most malignant primary brain tumors cannot be eradicated by surgery and need additional radiotherapy and chemotherapy.)
4. Treatment Monitoring
After initial treatment (such as surgery, radiation, or chemotherapy), continuous monitoring via imaging is crucial to assess the tumor’s response. For example, post-surgery MRIs can help detect whether the tumor has shrunk or if there is any recurrence. If the tumor hasn’t responded as expected or has recurred, doctors may adjust the treatment plan accordingly. This monitoring process helps ensure that the tumor remains under control and provides an early warning if the cancer recurs.
5. Differentiating Between Primary and Metastatic Tumors
Brain tumors can either be primary (originating in the brain) or metastatic (spread from cancer elsewhere in the body). The treatment strategies for these two types differ significantly. Medical imaging helps doctors identify the tumor’s origin, which is crucial for determining the best course of action. For instance, a metastatic tumor often appears differently on scans than a primary brain tumor, and understanding this difference allows doctors to tailor treatment to the specific needs of the patient. Knowing whether the cancer is primary or metastatic can greatly influence prognosis and therapeutic approaches, such as choosing between chemotherapy and targeted therapy.
If you’re experiencing persistent headaches or seizures, or you already have brain imaging results that need expert interpretation, our specialists are here to help. 👉 Upload your MRI or CT report for expert review on AI-PACS.
Why Are Different Imaging Modalities Used?
- MRI with and without contrast: The gold standard for brain tumor imaging, providing detailed views of soft tissues and tumor vascularity.
- Diffusion-Weighted Imaging (DWI) helps assess tumor cellularity and distinguish abscesses from tumors, while Susceptibility-Weighted Imaging (SWI) can detect hemorrhagic components and calcifications, aiding in tumor characterization.
- Magnetic Resonance Spectroscopy (MRS) can assess the tumor’s metabolic profile, helping differentiate between benign and malignant lesions.
- CT scan: Useful for detecting calcifications, hemorrhage and in emergency settings.
- Functional MRI (fMRI) and Diffusion Tensor Imaging (DTI): Helps map critical brain pathways before surgery.
- PET scan: Assesses metabolic activity, distinguishing high-grade from low-grade tumors.
Without proper imaging, misdiagnosis or delayed treatment can lead to significant complications, including neurological deficits and poor prognosis.
Explore Understanding T1-Weighted and T2-Weighted MRI Images to better interpret your MRI scans.
When Should Medical Imaging Be Used for Brain Tumor Diagnosis?
When Symptoms Suggest a Brain Tumor
Brain tumors can manifest with various neurological symptoms, including:
– Persistent or worsening headaches, especially in the morning
– Seizures, particularly new-onset in adults
– Vision problems, such as blurriness, double vision, or vision loss
– Weakness or numbness in limbs
– Cognitive and personality changes, including memory loss and confusion
– Difficulty with balance or coordination
Immediate imaging is warranted if any of these symptoms are progressive or unexplained.
When a Brain Tumor Is Suspected Clinically?
Patients with a history of cancer elsewhere in the body (e.g., lung or breast cancer) and new neurological symptoms should undergo urgent imaging to rule out metastatic disease.
When Monitoring Tumor Progression or Treatment Response?
Before treatment: Imaging determines the tumor’s exact location and characteristics.
Post-treatment follow-up: To assess tumor shrinkage or recurrence.
After surgery: Ensures complete resection and detects complications like bleeding or swelling.
When Planning for Neurosurgical Intervention
For tumors located near critical brain structures, advanced imaging like fMRI and tractography helps preserve essential functions during surgery.
Delaying imaging in symptomatic patients can lead to tumor progression, worsening prognosis, and reduced treatment options.
Who Needs Imaging and an Expert Consultation?
High-Risk Individuals Who Should Get Imaging
- Patients with persistent neurological symptoms: Unexplained seizures, headaches, or vision disturbances require prompt imaging.
- Individuals with a history of cancer: Metastatic brain tumors are common in patients with lung, breast, or melanoma cancers.
- People with a family history of brain tumors: Some genetic syndromes increase the risk of gliomas and meningiomas.
- Patients with known brain tumors: Regular imaging is essential for monitoring growth or response to therapy.
Read A Complete Guide to Reading Brain MRI for a step-by-step explanation of what radiologists look for.
Specialists Involved in the Imaging Process
- Neurologists: Evaluate symptoms and order initial imaging.
- Neurosurgeons: Plan surgical interventions based on imaging findings.
- Oncologists: Use imaging to guide chemotherapy or radiation therapy.
- Radiologists: Interpret scans and differentiate tumor types.
When to Seek a Second Opinion?
- Unclear or inconclusive imaging results
- Unique new sequences like MRS and FMRI … need an expert second opinion**
- Deciding between surgery, radiation, or chemotherapy
- Assessing treatment response or new symptoms post-treatment
A second opinion from an experienced radiologist can help avoid misdiagnosis and optimize treatment plans.
Conclusion
Brain tumors require timely and accurate diagnosis to improve treatment outcomes. Medical imaging is pivotal in early detection, surgical planning, and post-treatment monitoring. For expert interpretation of your medical imaging, use the radiology specialists from our team at AI-PACS for online reporting.
References: