Preparation for Breast MRI
Breast MRI for early detection of cancer, is a painless, non-invasive imaging method that uses radio waves and strong magnets to create highly detailed breast images. It serves as an adjunctive tool in breast cancer screening, capable of detecting abnormalities that may not be visible on mammography or ultrasound. Breast MRI is particularly beneficial for individuals with a confirmed breast cancer diagnosis who require a more thorough assessment. Depending on the patient’s clinical condition, breast MRI may be performed with or without a contrast agent like gadolinium, which helps enhance image clarity for better differentiation of tissues. The use of contrast enhances image clarity, allowing the radiologist to distinguish between normal and abnormal breast tissue more effectively.
Like other MRI procedures, breast MRI requires certain preparations:
- No special dietary or medication restrictions are needed before the scan.
- Inform the technician about any medical conditions, allergies, medications, tattoos, or claustrophobia.
- Wear comfortable clothing and remove all metallic objects, including jewelry, watches, credit cards, and hearing aids.
- If you have any metallic implants, consult with the imaging technician beforehand.
- To ensure clear imaging, take deep breaths and remain still during the scan.
- If contrast injection is required, fasting for at least four hours before the procedure is necessary.
- If you are pregnant or breastfeeding, inform the technician, as contrast agents are generally not recommended during pregnancy.
Need expert advice on your MRI preparation or report? Upload your MRI report to AI-PACS for professional review and personalized guidance.
Procedure and Positioning for Breast MRI
Upon entering the MRI room, the patient is positioned face down on a specialized table, with arms placed above the head. This positioning helps ensure optimal imaging by minimizing motion artifacts and allowing for better visualization of breast tissue. A device called a coil, designed with two hollow compartments, is placed under the breasts to stabilize them during imaging. The patient must remain completely still throughout the scan, as even minor movements can cause image distortion.
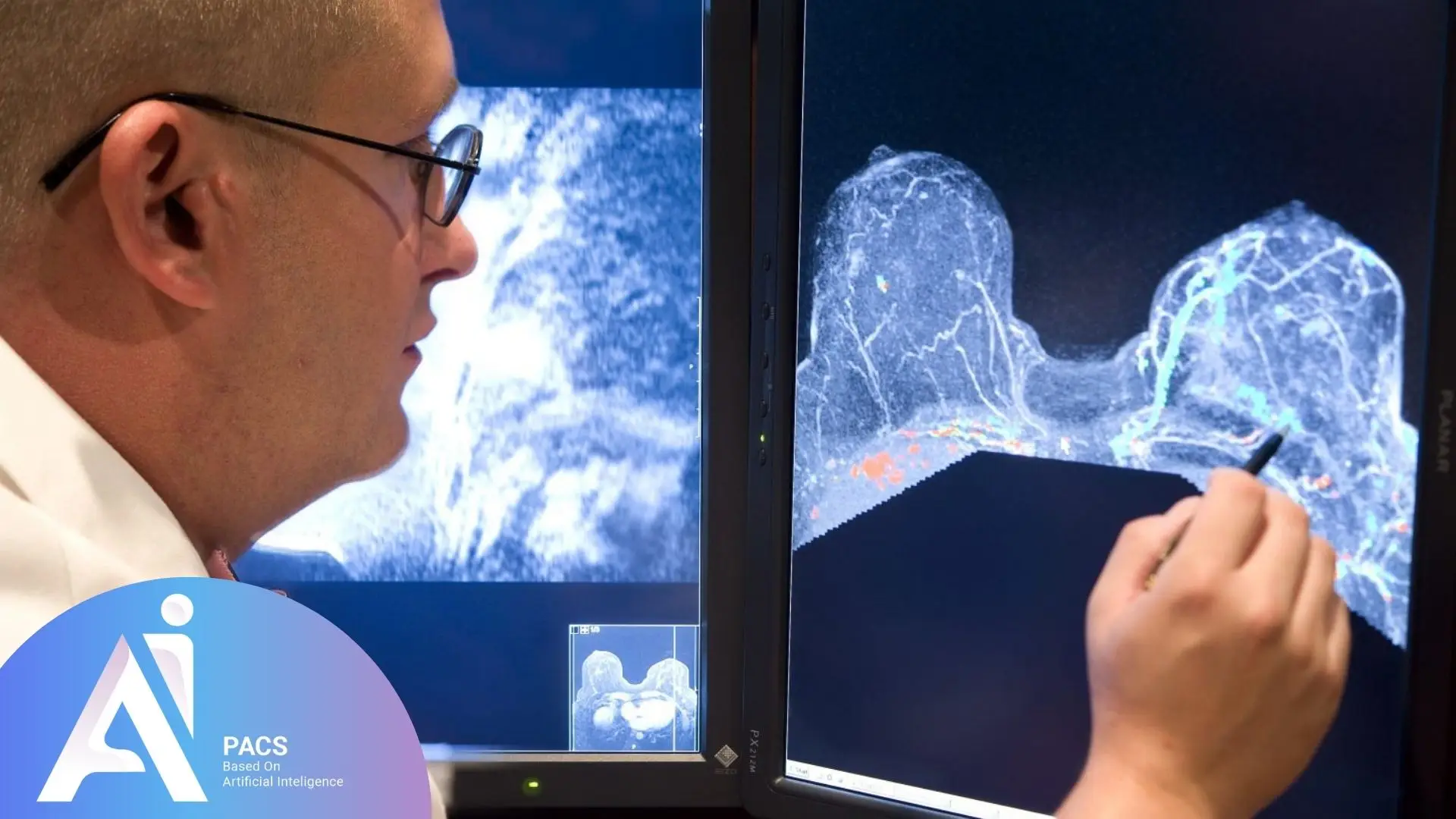
The technician maintains communication with the patient via a microphone and may instruct them to hold their breath momentarily to enhance image quality. The MRI system generates a series of cross-sectional images, which are then reconstructed into high-resolution 3D visuals. By applying a strong magnetic field, the scanner differentiates between various breast tissue types, aiding in the identification of abnormal masses.
Breast tumors typically have higher density and mass compared to surrounding normal tissues. Radiologists analyze these images from multiple angles, sometimes using a contrast agent like gadolinium for improved visualization of abnormalities. However, in some cases, contrast injection may not be necessary, and the physician will determine the best approach based on clinical indications.
Why is Breast MRI Performed?
The primary reasons for undergoing breast MRI include:
Detection of Breast Diseases
- Breast MRI is used to identify and assess tumors, cysts, and other abnormalities. It can distinguish between malignant and benign tissues, assisting physicians in diagnosing breast cancer.
Evaluation of Cancer Progression
- For patients diagnosed with breast cancer, MRI helps assess the extent of the disease and whether it has spread to surrounding tissues.
Monitoring Treatment Response
- Breast MRI is utilized to track treatment progress in patients undergoing chemotherapy or other cancer therapies, enabling doctors to assess tumor response, monitor changes in tissue structure, and adjust treatment plans as needed to improve outcomes.
Accurate Tumor Localization
- MRI provides precise tumor location and size measurements, including small and hard-to-detect lesions, aiding surgeons in planning tumor removal or radiation therapy.
Assessment of Lymph Node Involvement
- Breast MRI can evaluate lymph nodes to determine whether cancer has metastasized to these regions.
Screening for High-Risk Individuals
- Women with a family history of breast cancer or genetic mutations linked to increased cancer risk may undergo MRI as part of their routine screening program.
Systemic Changes and Benign Tumors
- MRI is used to assess endocrine changes in the breast and detect benign masses such as fibroadenomas.
Other Applications
- Young patients with dense breast tissue, especially those with a family history of breast cancer.
- Assessing cancer progression and tumor margins.
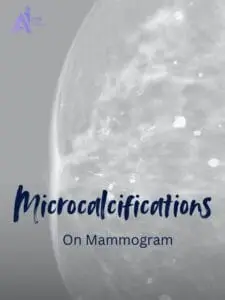
- Evaluating abnormalities that are difficult to detect on mammography.
- Supplementary breast imaging.
- Assessing breast implants, including silicone leakage detection.
- Screening high-risk women, particularly those with a strong family history of breast cancer.
- Simultaneous imaging of both breasts for comprehensive evaluation.
- Examining deeper chest and underarm tissues beyond breast tissue.
- Tracking treatment success after chemotherapy.
- Assessing tumor vascularization and its extent post-surgical removal.
Advantages of Breast MRI (MRM)
- The benefits of MRM include:
- Superior breast cancer detection accuracy.
- Non-invasive and radiation-free.
- Detection of multiple tumors.
- Pre- and post-treatment evaluation.
- Higher image resolution.
- Exceptional sensitivity and precision.
- A viable alternative to biopsy.
- Lower risk of allergic reactions compared to contrast agents used in CT scans and X-ray imaging.
Is Breast MRI Safe?
In general, breast MRI is a safe procedure with no significant reported risks. However, some potential concerns include:
- Patients must remain completely still, which can be challenging for individuals experiencing pain.
- The procedure may take a long time, which could be uncomfortable for some patients.
- Contrast injection may cause allergic reactions in certain individuals.
- Patients with claustrophobia may find the MRI environment distressing.
- Some individuals experience mild side effects such as headaches, nausea, dizziness, or warmth at the injection site, usually resolving within hours or days.
- Implant interference: Certain metallic implants may be affected by the magnetic field.
- Nephrogenic Systemic Fibrosis (NSF): Patients are screened for NSF risk before undergoing contrast MRI by evaluating kidney function through blood tests like serum creatinine levels and estimated glomerular filtration rate (eGFR). Those with severe kidney disease may need alternative imaging methods. Those with severe kidney disease may require alternative imaging methods to avoid potential complications. A rare but serious condition associated with gadolinium contrast in patients with severe kidney disease.
Already received your MRI report? Read our complete guide on understanding breast MRI and BI-RADS categories

Interpreting Breast MRI Results
Interpreting breast MRI requires high precision, as findings significantly impact treatment decisions. The reporting process involves:
Reviewing Medical History
- The radiologist examines the patient’s history, previous test results, and the reason for performing the MRI.
Analyzing Images
- The radiologist reviews the MRI scans across various cross-sections and angles. Both contrast-enhanced and non-contrast images are assessed for tissue abnormalities.
Identifying Tumors and Tissue Changes
- Suspicious masses, cysts, or abnormal tissue changes are carefully evaluated, including their size, shape, and characteristics.
BI-RADS Classification
- Breast MRI results are categorized using the Breast Imaging-Reporting and Data System (BI-RADS), which classifies findings on a scale from 0 to 6. Suspicious abnormalities may warrant further follow-up, such as a biopsy, for confirmation.
Reporting Findings
- A detailed report is prepared, outlining key findings and recommendations. The referring physician reviews these results to determine the next steps, such as additional tests or treatment.
At AI-PACS, our breast imaging experts provide second opinions to ensure that nothing important is overlooked. Getting a second opinion can provide you with peace of mind and ensure that you receive the best possible care. If you’ve received a breast MRI report and aren’t sure what the findings mean, upload it for expert interpretation.
👉 Upload your report now and get an expert review from our online radiology report services.
“Have you already done your breast MRI and received your report? Read our guide on how to interpret breast MRI terms and BI-RADS categories.
Final Thoughts
This article has provided an in-depth overview of breast MRI, its procedure, benefits, and comparisons with other imaging modalities. The selection of a breast imaging method depends on factors like age, family history, breast tissue density, and overall cancer risk. Consulting a physician is essential to determine the most appropriate imaging method based on individual health conditions. Patients should also discuss any personal risk factors, such as family history or existing medical conditions, to ensure the most effective screening approach. If you experience any unusual breast symptoms, seek medical advice promptly.
References: