Why Is Medical Imaging Needed for Traumatic Brain Injuries?
Imaging Traumatic Brain Injuries plays a pivotal role in the assessment of TBIs for several reasons:
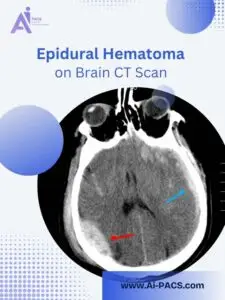
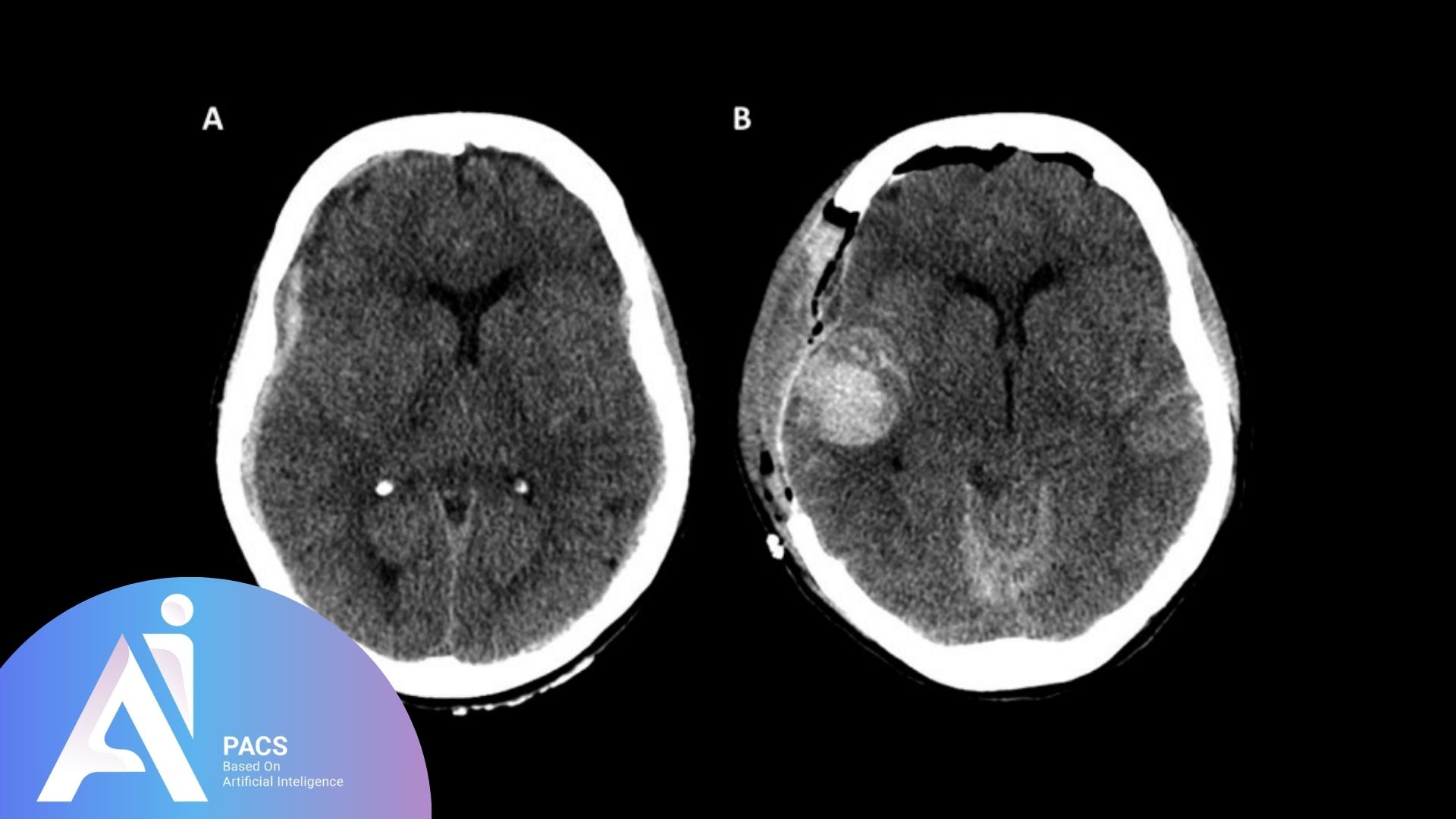
– Detection of Intracranial Hemorrhages: Identifying epidural or subdural hematomas that may require urgent intervention.
– Assessment of Skull Fractures: Evaluating fractures that could lead to complications such as infections or vascular injuries.
– Evaluation of Diffuse Axonal Injury (DAI): Detecting microscopic damage to white matter tracts may not be visible on standard imaging but can have significant clinical implications.
– Monitoring for Elevated Intracranial Pressure: Identifying signs of increased pressure within the skull that could necessitate surgical intervention.
– Detection of Cerebrospinal Fluid (CSF) Leaks: Identifying leaks that could lead to infections or other complications.
Common Patient Concerns:
– Why is imaging recommended? Imaging provides critical information about the extent and nature of the injury, guiding treatment decisions.
– What are the risks of missing a diagnosis without imaging? Undiagnosed injuries can lead to severe complications, including permanent neurological deficits or death.
– Why do some scans require contrast while others do not? Contrast agents enhance the visibility of specific structures and pathologies, aiding in a more accurate diagnosis.
If you’ve had a recent head injury and want clarity about your imaging results, our specialists can help. 👉 Upload your CT or MRI scan for expert review on AI-PACS.
Types of Imaging Used for Traumatic Brain Injuries
The two main imaging methods used for brain injuries are:
- CT (Computed Tomography) Scan:
Fast and highly effective at detecting acute bleeding and fractures. It’s usually the first choice in emergencies. - MRI (Magnetic Resonance Imaging):
It offers better detail of soft tissues and is more sensitive to subtle injuries, such as diffuse axonal injury (tiny tears in brain tissue). MRI is often used days or weeks after injury when symptoms persist.
When Should Medical Imaging Be Used for Traumatic Brain Injury Diagnosis?
The timing and urgency of imaging depend on the severity of the injury and the patient’s clinical presentation.
Immediate Imaging (Emergency Situations):
- Loss of Consciousness: Any period of unconsciousness following head trauma warrants immediate imaging.
- Neurological Deficits: Symptoms such as weakness, numbness, or speech difficulties necessitate prompt imaging.
- Severe Headache or Vomiting could be signs of intracranial hemorrhage or elevated intracranial pressure.
- High-Risk Mechanisms: Injuries resulting from high-speed collisions or falls from significant heights.
Recommended Imaging Modality: Non-contrast Computed Tomography (CT) scan is the first-line imaging modality in acute settings due to its rapid acquisition and high sensitivity for detecting acute hemorrhages and fractures.
Explore Increased Intracranial Pressure (ICP): Why, When, and Who Should Consider Imaging for insight into how imaging helps detect brain swelling after trauma.
Delayed Imaging (Non-Emergent Situations):
– Persistent or Worsening Symptoms: Ongoing headaches, dizziness, or cognitive changes after the initial injury.
– Suspected Diffuse Axonal Injury: Patients with a history of traumatic injury presenting with cognitive or behavioral changes.
– Evaluation of Chronic Symptoms: Assessment of long-term complications such as post-traumatic epilepsy or chronic headaches.
Recommended Imaging Modality: Magnetic Resonance Imaging (MRI) is preferred for evaluating subacute or chronic injuries due to its superior soft tissue contrast and ability to detect diffuse axonal injuries.
Who Needs Imaging and an Expert Consultation?

Patients with Red Flag Symptoms: Individuals presenting with severe headaches, seizures, focal neurological deficits, or altered mental status should undergo immediate imaging.
– Elderly Patients: Older adults are at higher risk for subdural hematomas, even with minor head trauma, due to brain atrophy and anticoagulant use.
– Patients on Anticoagulant Therapy: These individuals have an increased risk of bleeding, necessitating a lower threshold for imaging.
– Individuals with Recurrent Head Injuries: Repeated trauma can lead to cumulative damage, such as chronic traumatic encephalopathy (CTE), requiring thorough evaluation.
Specialists Involved in TBI Imaging and Care
- Emergency physicians stabilize patients and decide on urgent imaging
- Radiologists interpret scans and highlight findings
- Neurologists manage ongoing neurological issues
- Neurosurgeons intervene surgically when necessary
The Importance of Second Opinions
Given the complexity of TBIs and Imaging Traumatic Brain Injuries, obtaining a second opinion can be invaluable, especially for complex cases or when considering surgical interventions. Platforms like AI-PACS.com offer expert consultations, ensuring accurate interpretations and optimal management plans. Also, Learn more about Epidural Hematoma and Brain CT Diagnosis to understand how imaging detects life-threatening bleeding.
If you or a loved one has experienced a head injury and requires an expert second opinion on imaging studies, for quick and accurate TBIs reporting, visit our online radiology report services page today!
References
National Library of Medicine. “Traumatic Brain Injury.”
PMC. “Imaging in Traumatic Brain Injury.”