Understanding Increased Intracranial Pressure (ICP): Causes, Symptoms, and the Importance of Brain Imaging
Increased pressure inside the skull can be life-threatening. The skull is a closed space, so any change in brain tissue, blood flow, or cerebrospinal fluid (CSF) can raise intracranial pressure (ICP). Detecting this early is not just critical, it can be life-saving.
Several conditions can cause increased intracranial pressure (ICP), and imaging plays a crucial role in not just detecting but also identifying the underlying cause, providing you with the reassurance and information you need.
Need expert interpretation of your brain imaging? 👉 Upload your MRI or CT scan for professional review now
Why Is Imaging Important for Increased Intracranial Pressure?
Imaging, especially brain MRI or CT, helps detect the causes of raised ICP and prevent long-term damage.
Common Causes of Increased ICP:
- Venous sinus thrombosis (CVST): More common in women, especially those on oral contraceptives (OCPs) or with clotting risks like DVT. This can lead to impaired venous drainage and raised pressure.
- Idiopathic Intracranial Hypertension (IIH): A condition seen mostly in young overweight women, with no visible mass or hydrocephalus on imaging, but increased pressure is present.
- Brain tumors or mass lesions: Space-occupying lesions increase pressure inside the skull.
- Obstructive hydrocephalus: Blocked CSF flow leads to enlarged ventricles and ICP elevation.
- Normal-pressure hydrocephalus (NPH) is seen in older adults. Despite normal CSF pressure, patients have impaired absorption or flow symptoms.
When Should Brain Imaging Be Performed for Suspected ICP?
Symptoms of increased intracranial pressure (ICP) may develop gradually or suddenly. Imaging helps confirm the diagnosis and guide treatment.
Clinical Signs That Suggest Raised ICP:
- Persistent or worsening headaches (especially in the morning)
- Nausea and vomiting
- Blurred vision or double vision
- Papilledema (swelling of the optic disc seen on fundus exam)
- Altered consciousness or confusion
- Seizures, in some cases
Imaging Findings May Include:
- Flattening of the posterior globe (in IIH)
- Empty sella (in IIH)
- Enlarged ventricles (in NPH or hydrocephalus)
- Venous filling defects on MRV or CTV in venous sinus thrombosis
- Mass lesions causing midline shift or edema
Who Needs Brain Imaging and Expert Consultation?
Patients with any signs of increased intracranial pressure (ICP) should receive prompt brain imaging and clinical evaluation.
High-Risk Groups:
- Women taking oral contraceptive pills (OCPs), which are hormone-based medications used for birth control, or those with known clotting disorders
- Young women with chronic headache and vision symptoms (suspect IIH)
- Elderly patients with memory loss, urinary incontinence, and gait problems (triad of NPH)
Clinical Evaluation Also Includes:
- Ophthalmoscopy to check for papilledema
- Neurological exam to assess mental status and motor function
- CSF pressure measurement via lumbar puncture (if no mass effect is seen on imaging)
AI-PACS Is With You
Have an unclear diagnosis? Do you need an expert review of brain imaging?
At AI-PACS.com, our radiologists offer fast and accurate second opinions on MRI and CT scans for suspected increased intracranial pressure (ICP) and related conditions.
You can upload your scan securely and receive detailed feedback.
🖥️ If you already have your imaging and need it interpreted quickly and professionally, check out our Online Reporting Services to get expert insights, without delays or extra clinic visits.
Deeper Dive Into Brain Imaging for ICP (clear, not overly technical)
Choosing the right test
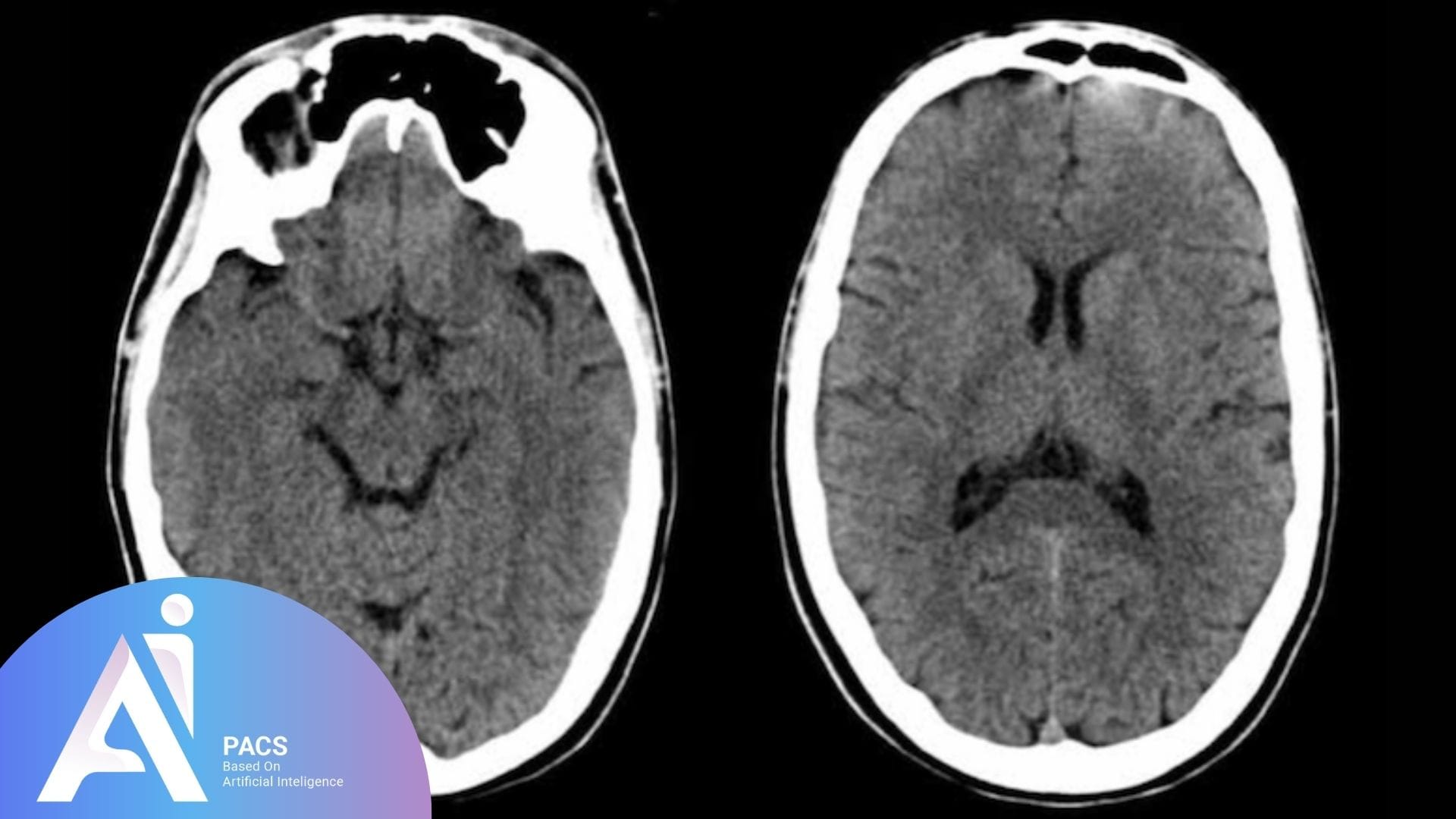
• CT head is fast. It helps in emergencies to exclude bleeding and major mass effect and can suggest hydrocephalus.
• MRI brain shows soft tissues, optic nerves, and posterior fossa in detail and is preferred when available.
• MRV or CTV evaluate the venous sinuses when thrombosis is suspected. The choice depends on urgency and local expertise [1][3].
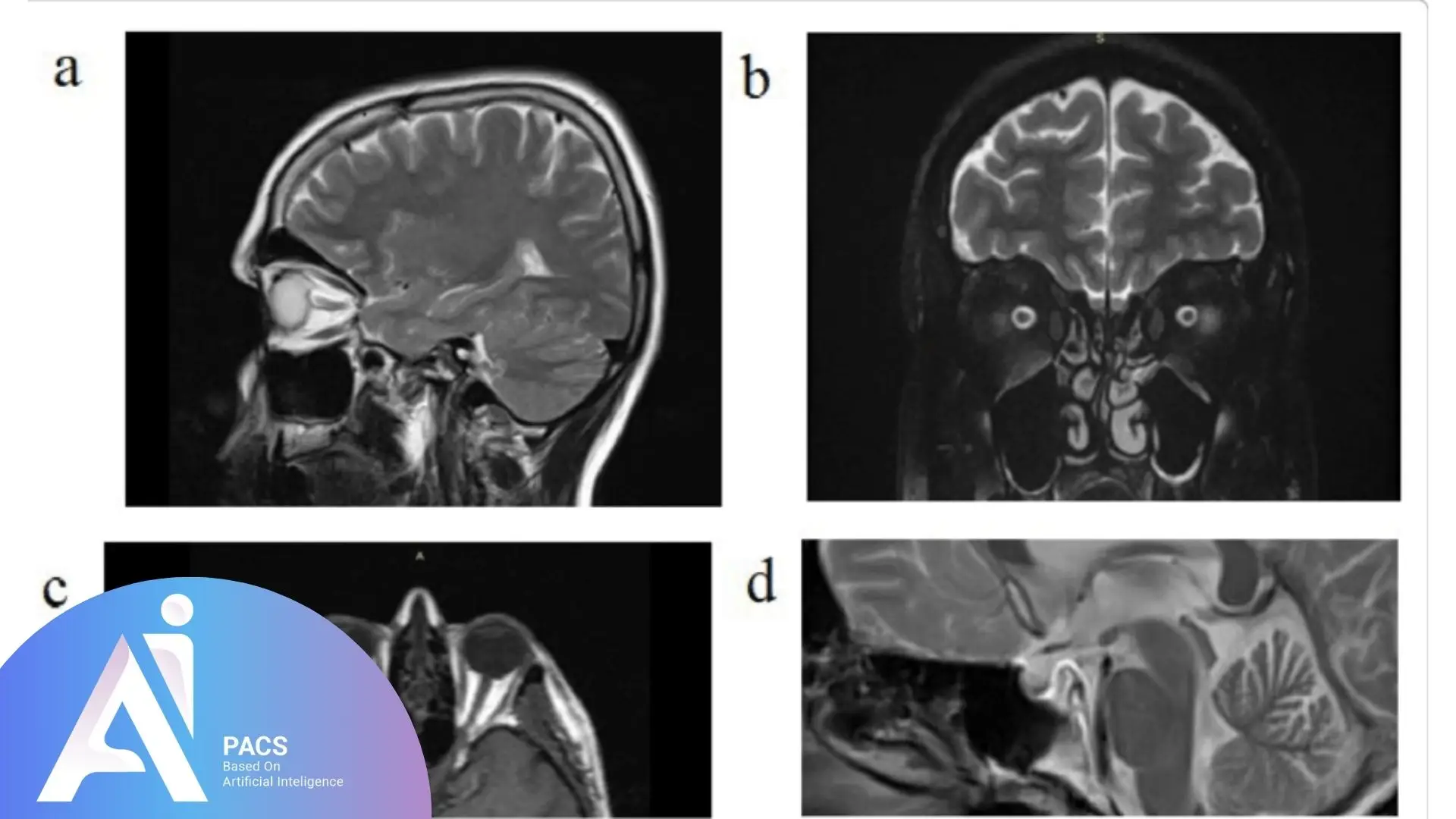
Idiopathic intracranial hypertension (IIH)
Imaging is often normal in the brain itself, but several signs support the diagnosis when a mass has been excluded: posterior globe flattening, enlarged optic nerve sheaths, partially empty sella, and transverse sinus narrowing. MRI with MRV is recommended to exclude secondary causes and document these features. Diagnosis then relies on a lumbar puncture showing elevated opening pressure after imaging confirms it is safe [2][6].
Cerebral venous sinus thrombosis (CVST)
Clots in the dural venous sinuses impair brain drainage and raise pressure. Symptoms range from headache to vision loss and seizures. MRV or CTV shows a filling defect or lack of normal flow. Early recognition matters because treatment with anticoagulation improves outcomes, even when hemorrhage is present in selected cases [3].
Hydrocephalus and normal‑pressure hydrocephalus (NPH)
Obstruction of CSF flow enlarges the ventricles and elevates pressure. In older adults with the triad of gait change, cognitive issues, and urinary symptoms, imaging can suggest NPH. Radiologists describe ventriculomegaly, the Evans index, callosal angle, and a pattern called DESH. MRI is usually appropriate; CT can also confirm ventriculomegaly. Findings help select patients for CSF drainage trials and shunt planning [4].
Mass lesions and edema
Tumors, abscesses, and hemorrhages can raise pressure through mass effect and swelling. Imaging shows midline shift, compressed ventricles or cisterns, and herniation patterns. These guide urgent therapies such as steroids, surgery, or CSF diversion and shape discussions about timing and risk [1][5].
What the Report Means & Next Steps
Your report should answer three questions: what is causing the pressure, how severe the effects are, and what to do next. Look for terms like ventriculomegaly, midline shift, herniation, sinus thrombosis, empty sella, optic nerve sheath dilation, or posterior globe flattening. Ask your clinician whether additional tests are needed, when to repeat imaging, and how the plan protects vision and brain function [1][2][4].
Final Thoughts
Increased intracranial pressure is a serious issue. Causes range from clots and tumors to conditions like IIH and NPH. Clinical signs may be subtle at first, so early imaging is key.
MRI and CT help detect the cause, guide treatment, and prevent long-term damage. Patients and doctors can act fast and confidently with expert reviews from AI-PACS.
References
- American College of Radiology. ACR Appropriateness Criteria: Headache. https://acsearch.acr.org/docs/69482/Narrative/
- American College of Radiology. ACR Appropriateness Criteria: Pseudotumor Cerebri Syndrome (Idiopathic Intracranial Hypertension). https://acsearch.acr.org/docs/69439/Narrative/
- Saposnik G, et al. Diagnosis and Management of Cerebral Venous Thrombosis. AHA/ASA Scientific Statement. Stroke. 2024;55:e77–e126. https://pubmed.ncbi.nlm.nih.gov/38284265/
- American College of Radiology. ACR Appropriateness Criteria: Dementia (includes suspected NPH). 2024 update. https://acsearch.acr.org/docs/3111292/Narrative/
- RSNA/ACR. RadiologyInfo.org. Brain MRI. https://www.radiologyinfo.org/en/info/mri-brain
- Sarrami AH, et al. Idiopathic intracranial hypertension: Imaging approaches and the role of MRV. Insights Imaging. 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC10162046/
Disclaimer: This article is educational and not a substitute for medical care.