Why Is Imaging Important in Musculoskeletal Conditions?
MSK imaging helps in three major clinical settings:
1. Sports Medicine Injuries (Professional Athletes)
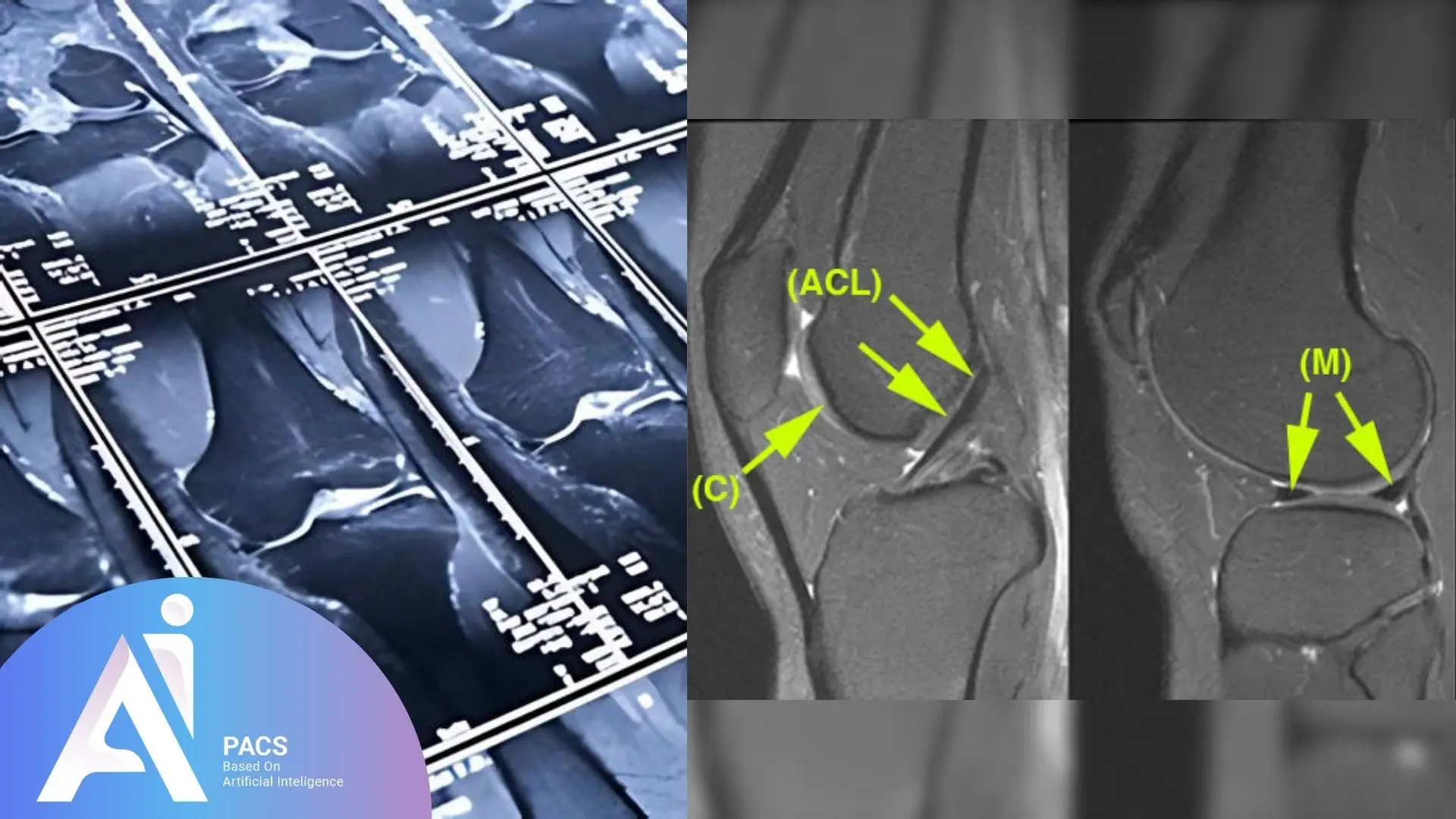
Professional athletes often suffer acute injuries during training or competition. These injuries can include ligament tears, tendon damage, or joint dislocations.
- Imaging (especially MRI) is needed quickly to confirm the diagnosis
- Early diagnosis enables targeted treatment and rehabilitation
- The goal is a rapid return to sport, as performance is their profession
Explore this more on our sports medicine page.
2. Repetitive or Chronic Joint Injuries (Non-Athletes, Over Age 35–40)
These patients are not professional athletes but often stay active through work or recreational sports. Over time, minor repetitive injuries can lead to:
- Joint pain and swelling
- Tendinosis, bursitis, or cartilage degeneration
- Decreased joint function and range of motion
Imaging can detect:
- Micro-tears in tendons
- Joint space narrowing or cartilage wear
- Early degenerative changes before severe damage occurs
3. Inflammatory and Infectious Joint Disorders
Autoimmune and infectious conditions can silently destroy joints unless detected early.
- Rheumatoid arthritis causes synovial inflammation and joint erosion
- Septic arthritis or viral arthritis can result in rapid joint damage
Imaging is crucial because:
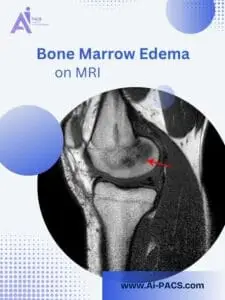
- MRI and ultrasound detect early synovitis, bone edema, or effusion
- Early diagnosis = better outcomes and can prevent joint replacement surgery
When Should Musculoskeletal Imaging Be Performed?
Knowing when to image makes a difference in outcomes.
Imaging Should Be Considered When:
- Pain lasts more than a few weeks or is disabling
- There’s limited motion or clicking in the joint
- Trauma or sports injury occurred
- Inflammatory arthritis is suspected (e.g., morning stiffness, multiple joints)
- Fever, redness, or infection signs suggest septic arthritis
Imaging Modalities Used:
- X-rays: First step for bone injuries or arthritis
- Ultrasound: For soft tissue and fluid collection
- MRI: Best for cartilage, tendons, ligaments, and early inflammation
- CT scan: For bone detail and complex fractures
Who Should Get Imaging and Expert Consultation?
Early and accurate MSK imaging brings relief and reassurance to professional athletes, active adults, and patients with suspected inflammation or infection.
Imaging Is Especially Important For:
- Athletes needing fast recovery
- Middle-aged patients with chronic joint stress
- Patients with autoimmune conditions like rheumatoid arthritis or lupus
- Anyone with red flag symptoms like joint locking, fever, or rapid progression
AI-PACS, our advanced imaging platform, connects you with radiology experts who understand sports medicine, inflammatory conditions, and degenerative joint disease. It’s not just about taking pictures, it’s about accurate, expert interpretation that helps your care team make better decisions.
What The Report Means & Next Steps
Your report should answer three questions: what structure is abnormal, how severe is it, and what management is recommended. Look for clear terms like partial or full‑thickness tear, effusion, synovitis, bone bruise, or osteoarthritis grade. Ask your clinician how the imaging fits your symptoms and exam, whether activity modification or therapy is enough, and when to consider injections or surgery. Imaging informs decisions, but your goals and function guide the final plan.
AI-PACS Is With You
MSK imaging isn’t just about taking pictures. It’s about accurate, expert interpretation that supports your care team in making better decisions for you.
At AI-PACS.com, we offer online radiology second opinions; fast readings for MRI, ultrasound, and CT scans focused on joints, tendons, and soft tissue injuries.
Deeper Dive Into Imaging (clear, not overly technical)
Start with radiographs when bone is the question
X‑rays are fast and affordable. They show fractures, dislocations, and arthritis patterns. In many pathways, radiographs come first for traumatic knee or shoulder pain, and also for persistent, non‑traumatic knee pain before advanced tests are added [1][6].
Ultrasound: dynamic views and guided care
Ultrasound uses sound waves to show tendons, bursae, and fluid. It can reveal rotator cuff tears, tennis elbow changes, and inflammatory synovitis, which is swelling of the joint lining. Because it is dynamic, the sonographer can watch structures move and can guide precise injections or aspirations during the same visit. Ultrasound is especially helpful for hands, shoulders, and ankles, and it avoids radiation [2][4].
MRI: the detail king for soft tissues and early inflammation
MRI excels at seeing cartilage, menisci, labrum, ligaments, bone marrow edema, and nerve entrapment. It often clarifies why pain persists when X‑rays are normal. In inflammatory arthritis, MRI can detect active synovitis and early erosions before damage is obvious on radiographs, which can change therapy sooner [2][4].
CT and 3D planning when bone detail matters
CT shows complex fractures, small bone fragments, and osteoid lesions with exquisite detail. It helps plan surgery around the shoulder, hip, and ankle and is useful when metal hardware limits MRI. For suspected infection where MRI is contraindicated, CT and nuclear medicine studies can contribute to the diagnosis alongside lab tests and aspiration [5].
Inflammatory and infectious joints need early imaging plus aspiration
Autoimmune diseases like rheumatoid arthritis inflame the synovium. Ultrasound and MRI detect this early and can track response to therapy. Suspected septic arthritis is an emergency. Imaging can show effusion and neighboring bone changes, but joint aspiration for culture remains the decisive step that directs antibiotics and surgical washout [4][5].
Final Thoughts
In this new musculoskeletal series, we’ll cover joints one by one, starting with the shoulder, knee, hip, spine, and more.
Whether you’re an active adult or experiencing joint pain due to inflammation or infection, remember, you play a crucial role in your diagnosis and treatment planning. With expert insight from the AI-PACS team, we’re here to support your movement and recovery.
With expert insight from AI-PACS team, we’re here to support your movement and recovery.
References
- American College of Radiology. ACR Appropriateness Criteria: Chronic Knee Pain. https://acsearch.acr.org/docs/69432/Narrative/
- org. Musculoskeletal MRI. https://www.radiologyinfo.org/en/info/muscmr
- American College of Radiology. ACR Appropriateness Criteria: Acute Shoulder Pain. https://acsearch.acr.org/docs/69433/narrative/
- Mandl P, et al. 2023 EULAR recommendations on imaging in diagnosis and management of rheumatoid arthritis. Ann Rheum Dis. 2024;83:752–764. https://ard.bmj.com/content/83/6/752
- American College of Radiology. ACR Appropriateness Criteria: Suspected Osteomyelitis, Septic Arthritis, or Soft Tissue Infection. https://acsearch.acr.org/docs/3094201/Narrative/
- American College of Radiology. ACR Appropriateness Criteria: Acute Trauma to the Knee. https://acsearch.acr.org/docs/69419/narrative/
Disclaimer: This article is educational and not a substitute for medical care.