Understanding Posterior Fossa Masses: Why Imaging Is Key to Early Diagnosis and Treatment
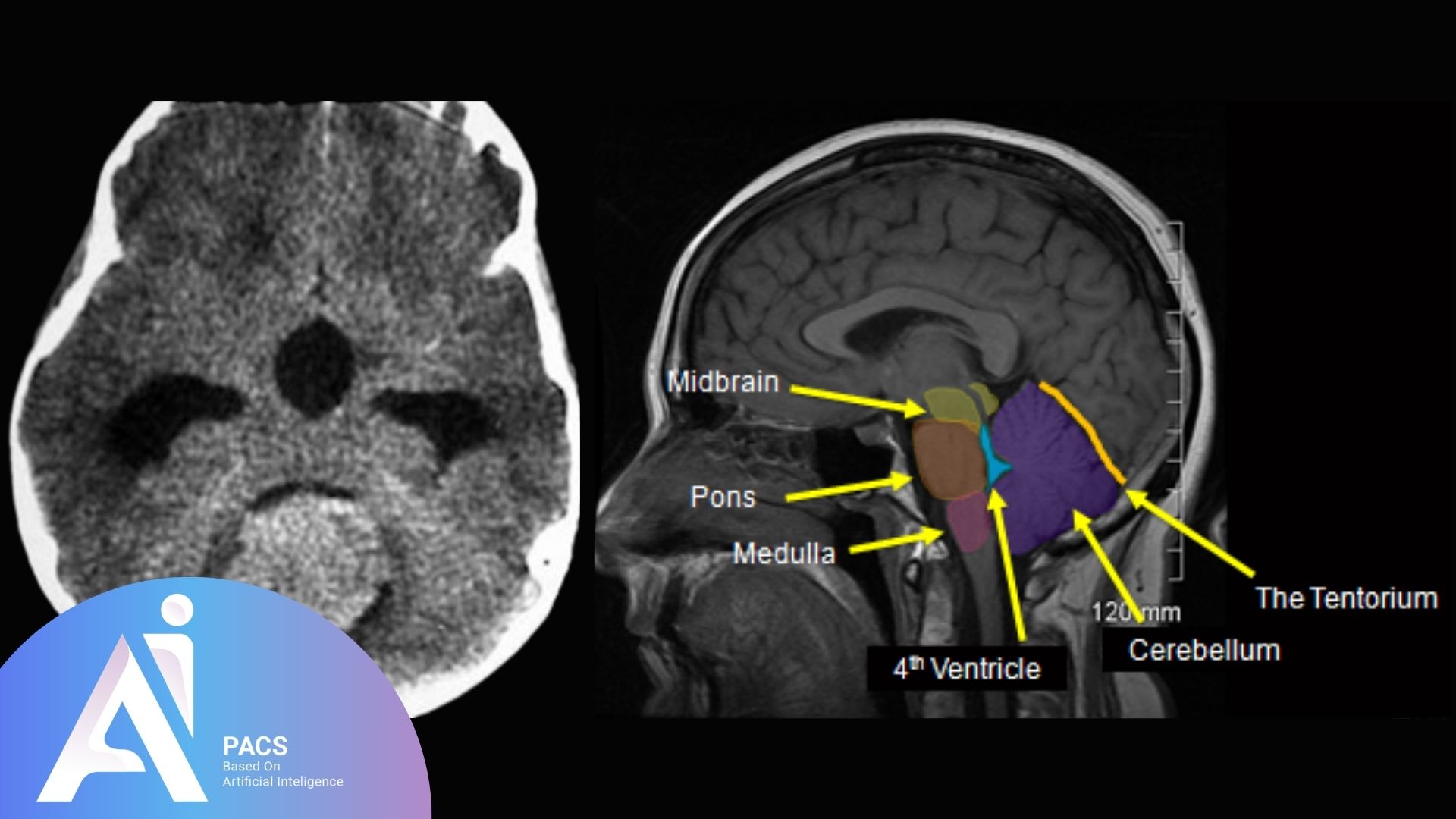
The posterior fossa sits at the back of the skull and houses the cerebellum and brainstem. These structures control balance, coordination, breathing, and heart rate. Because the space is tight, even a small mass or swelling can raise pressure quickly and produce serious symptoms. MRI gives the clearest view of this area and often detects problems that other tests miss.
Early, accurate imaging matters. It helps confirm what is causing symptoms, shows whether fluid is backing up in the brain’s ventricles, and guides a safe plan with the care team. In many cases, timely MRI changes the next step from waiting to treating.
Masses in the posterior fossa can be particularly hazardous due to the limited space and the presence of vital structures in this area. The posterior fossa is located at the back of the skull and contains the cerebellum and brainstem, which control balance, coordination, and vital body functions.
When pressure builds up in this region, it can quickly affect the midbrain, leading to serious symptoms and even life-threatening complications. That’s why early and accurate imaging, especially with MRI, is critical.
Experiencing dizziness, unsteady balance, or morning headaches? 📁 Upload your brain MRI or CT scan now for expert review
Why Is Imaging Important for Posterior Fossa Lesions?
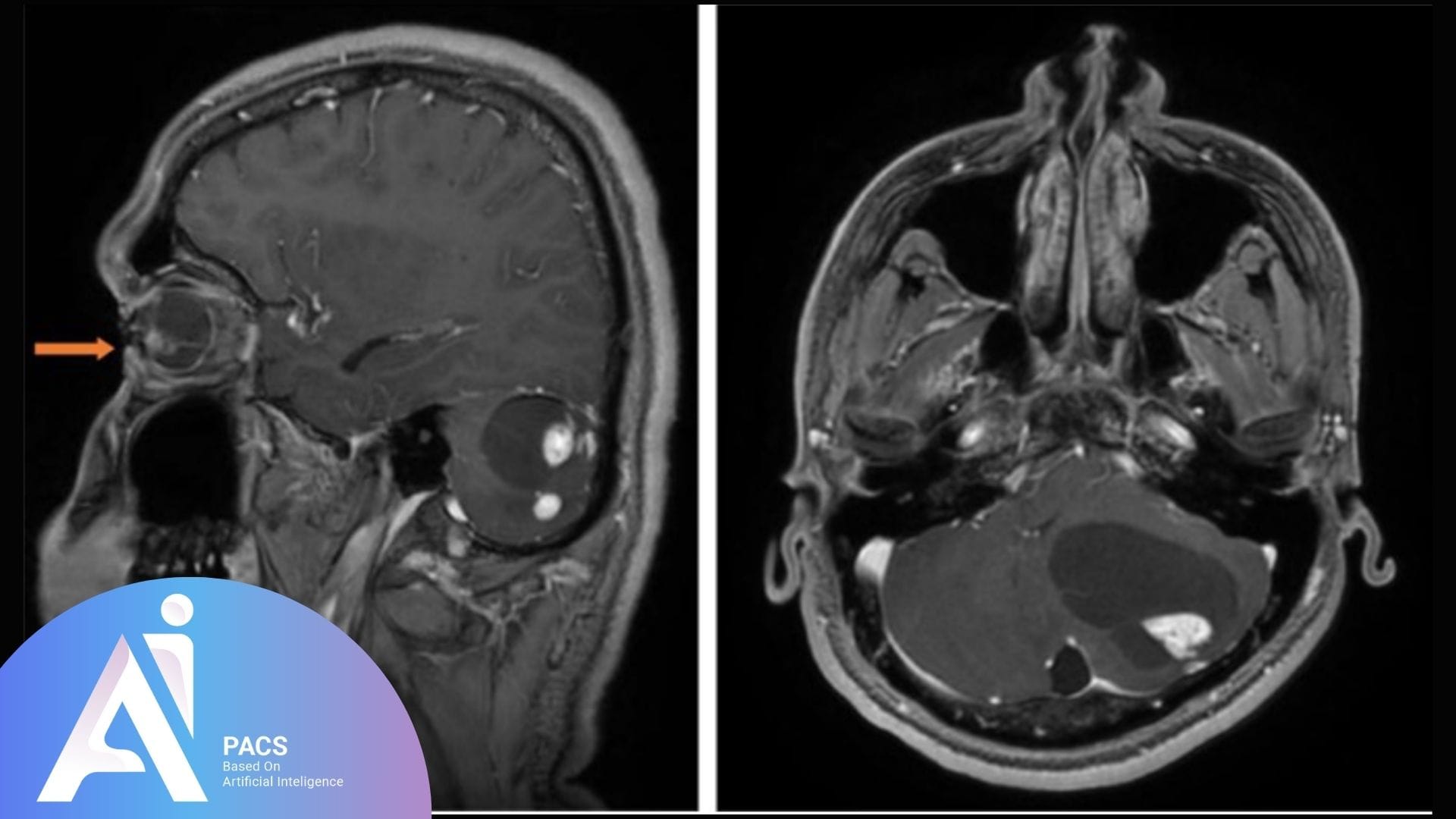
MRI helps detect and define masses in the posterior fossa. It shows the size of the lesion, its location, and how it affects nearby brain structures.
What Can MRI Reveal?
- Tumors like juvenile pilocytic astrocytomas (common in children)
- Hemangioblastomas (seen more in adults)
- Metastases or primary brain tumors in older patients
- Cysts or vascular malformations
MRI with contrast can also help determine if the mass is growing, pressing on nearby areas, or causing hydrocephalus (a condition where fluid builds up).
Why the Posterior Fossa Is High-Risk
- It’s a small, tight space. Even a small lesion can raise pressure.
- The cerebellum plays a crucial role in maintaining balance and coordination.
- The brainstem controls breathing, heart rate, and alertness.
- Swelling or pressure in this area can affect the midbrain rapidly.
Without imaging, these problems might be missed until symptoms become severe.
When Should Imaging Be Done for Posterior Fossa Symptoms?
Time is of the essence. Early symptoms may be subtle, but a prompt diagnosis can prevent potential brain damage.
Signs That Need Urgent MRI:
- Headaches, especially in the morning or with vomiting
- Unsteady walking or clumsiness
- Blurred vision or double vision
- Dizziness or vertigo
- Nausea with no apparent cause
- Changes in behavior or alertness
Symptoms in Children:
- Balance problems
- Delay in motor skills
- Persistent vomiting
- Head tilt or abnormal eye movements
Don’t wait if you’re noticing persistent headaches or coordination issues. Consult AI-PACS experts for fast and accurate imaging interpretation.
Who Should Get Imaging and Expert Review?
Children and older adults are at particular risk. Different types of tumors are more common in each group:
Common Posterior Fossa Tumors by Age Group:
- Children: Pilocytic astrocytoma, medulloblastoma, ependymoma
- Adults: Hemangioblastoma, metastases, cerebellar glioma
Specialists Involved:
- Pediatricians or neurologists for children
- Neurosurgeons for surgical planning
- Radiologists for detailed MRI interpretation
- Oncologists, if cancer is suspected
Early imaging enables better planning and often results in improved outcomes.
AI-PACS Is With You
AI-PACS, an advanced AI-powered platform, is designed to assist medical professionals in interpreting medical images. It can help in the early detection and accurate diagnosis of posterior fossa lesions, ensuring timely and effective treatment.
If you or a loved one is experiencing symptoms related to posterior fossa lesions, seeking a second opinion can provide reassurance and guide the next steps.
At AI-PACS.com, our experts provide fast and trusted reviews of brain MRI and CT scans.
Need a second opinion now?
📁 Submit your report for a review by an expert in order to obtain detailed feedback.
Deeper Dive Into Imaging (clear, not overly technical)
MRI or CT: which first?
MRI is usually preferred for the posterior fossa because it shows soft tissues in high detail and is less affected by bone. CT is faster and can help if there is trauma or bleeding, but CT is less sensitive than MRI for many posterior fossa problems. In children, teams use pediatric protocols and consider quick MRI techniques to reduce the need for sedation. [1][4]
What contrast adds
Gadolinium contrast makes active lesions stand out and helps differentiate tumor from inflammation or infection. Radiology teams check kidney function and allergy history before contrast and use it only when it can change care. [1][2]
Typical causes by age
Patterns vary with age. In children, common posterior fossa tumors include medulloblastoma, ependymoma, and circumscribed astrocytomas such as pilocytic astrocytoma. In adults, causes include metastases and, less often, hemangioblastoma or cerebellar glioma. Your radiologist uses the lesion’s location, signal, and enhancement to guide the differential list and next steps. [2][5]
Advanced MRI that guides treatment
Beyond routine T1 and T2 images, diffusion‑weighted imaging can flag cellular tumors, perfusion imaging can estimate tumor blood volume, and MR spectroscopy can sample tumor chemistry. Diffusion tensor imaging and functional MRI help surgeons plan approaches that avoid critical pathways. [2]
Watching for complications
Any mass in the posterior fossa can block cerebrospinal fluid outflow and cause hydrocephalus. MRI shows ventricle size and CSF flow, which helps teams decide on urgent measures such as external drainage or shunt in selected cases. [6]
What The Report Means & Next Steps
Your report should answer three questions: where the lesion sits, what it most likely represents, and whether there is pressure on nearby structures or fluid buildup. Ask your clinician how the imaging matches the exam, whether steroids or surgery are needed, and what the safe timeline is for action. If the diagnosis is uncertain, a short‑interval follow‑up MRI or a targeted biopsy may be advised.
Already have your MRI or CT scan report? Upload it for a professional review and ensure you understand every detail before making treatment decisions
Final Thoughts
Posterior fossa lesions are serious. Even small changes can be dangerous because the space is limited, and the structures are vital.
MRI is the most effective tool for detecting problems early. If you notice symptoms or if your child shows balance or behavior changes, please don’t wait. Trust in the power of imaging. Trust in the expert reviews from AI-PACS to help guide you towards the best possible care.
References
- RSNA/ACR RadiologyInfo.org. Brain MRI. https://www.radiologyinfo.org/en/info/mri-brain
- American College of Radiology. ACR Appropriateness Criteria: Brain Tumors. https://acsearch.acr.org/docs/3195155/Narrative
- NICE Quality Standard QS198. Headaches and red‑flag symptoms in children. https://www.nice.org.uk/guidance/qs198/chapter/Quality-statement-1-Headaches-and-red-flag-symptoms-in-children
- ACR Appropriateness Criteria: Ataxia‑Child. https://acsearch.acr.org/docs/3158172/Narrative
- NCI PDQ. Childhood Medulloblastoma and Other CNS Embryonal Tumors. https://www.cancer.gov/types/brain/hp/child-cns-embryonal-treatment-pdq
- Hydrocephalus. https://www.ninds.nih.gov/health-information/disorders/hydrocephalus
Disclaimer: This article is educational and not a substitute for medical care.