Understanding Visual Disturbances: Why Medical Imaging Is Crucial for Diagnosis
Vision changes can be unsettling. They might appear in an instant or creep up over months. Some causes are minor and temporary. Others involve the eye, the optic nerve that carries signals, or the brain areas that process sight. The only way to see inside these structures is with medical imaging.
Your visual pathway starts at the eyeball, runs through the optic nerves and chiasm where fibers cross, then continues along optic tracts and radiations to the occipital lobes. A problem anywhere along this route can blur, dim, or distort what you see. MRI and CT help pinpoint the source so that the right treatment can begin without delay.
The visual pathway begins at the globe (eyeball) and terminates in the brain’s occipital lobe. Signals pass through the optic nerve, optic chiasm, optic tracts, and optic radiations. Damage in any of these parts can affect vision.
Sudden or persistent vision changes shouldn’t wait. 📁 Upload your brain or orbital MRI for expert review today
Why Is Imaging Important for Vision Problems?
Medical imaging, by revealing what’s happening inside the eye and brain, provides a sense of relief to patients, helping doctors find the cause of visual symptoms.
What Can Imaging Detect?
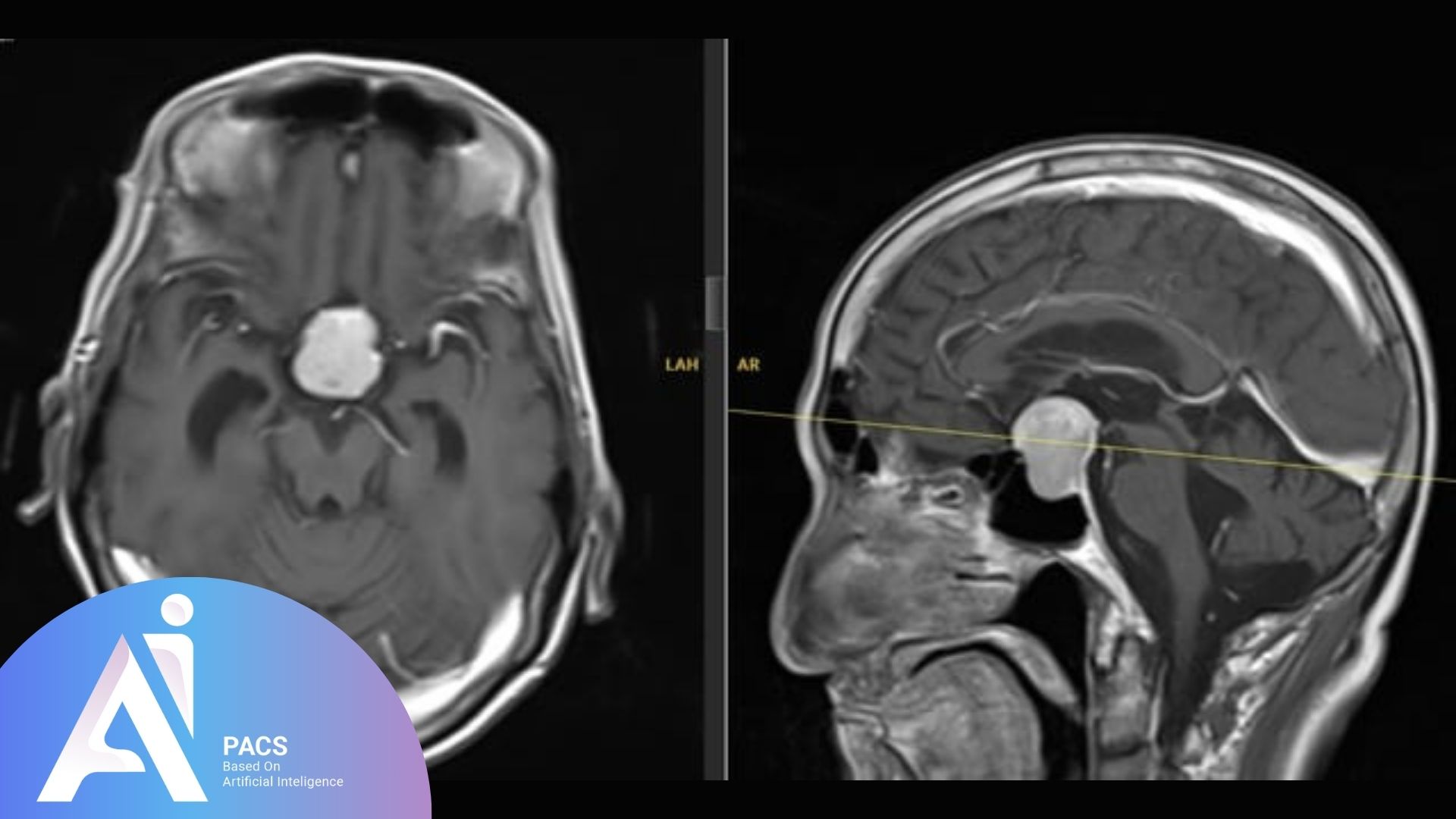
- Tumors pressing on the optic nerve
- Inflammation like optic neuritis
- Stroke or bleeding near the visual areas
- Damage to the occipital lobe
- Multiple sclerosis (MS)
- Trauma after head injury
Why Do Some Patients Need Contrast?
Contrast helps show specific problems more clearly, such as inflammation, tumors, or blood vessel issues. Your doctor will determine the course of treatment based on your symptoms.
When Should You Get Medical Imaging for Vision Issues?
The timing depends on your symptoms. Some people need imaging right away. Others may be monitored first.
Urgent Signs That Need Imaging:
- Sudden loss of vision
- Pain with eye movement
- New or ongoing double vision
- Vision problems with headache or weakness
- Vision loss after a fall or injury
When Imaging Can Wait:
- Gradual changes in vision
- Recurrent blurry vision without other symptoms
- Known conditions under regular follow-up (e.g. MS)
Who Needs Imaging and Expert Review?
Not everyone with eye symptoms needs a scan. But for some, it’s critical.
Patients Who Should Consider Imaging:
- Anyone with sudden or severe vision changes
- People with diabetes, MS, or autoimmune disease
- Children with unusual vision symptoms
- Patients with visual field loss (e.g., tunnel vision or blind spots)
Specialists Involved:
- Family doctors for the first check
- Ophthalmologists for eye exams
- Neurologists, if the brain or nerves are involved
- Radiologists to interpret MRI or CT scans
AI-PACS Is With You
Understanding imaging results can be challenging. However, with the right knowledge, you can seek a second opinion with confidence, ensuring you have a clear understanding of your condition.
At AI-PACS.com, expert radiologists are simply available to review your MRI or CT scans, providing clear feedback and support when you need it most.
Need a second opinion?
If you’re seeking reliable online radiology report services, AI-PACS is here to provide you with the best second opinion on your medical images, delivered by our team of expert radiologists.
📁 Submit your report for a review by an expert in order to obtain detailed feedback.
Deeper Dive Into Imaging (clear, not overly technical)
Choosing the right test: MRI vs CT
MRI is usually the first choice for optic nerve, chiasm, and brain causes of visual disturbance because it shows soft tissues in high detail. CT is faster, widely available, and best for acute bleeding and bone injury. In many emergency rooms, a rapid head CT is done first to exclude hemorrhage, followed by MRI if needed to evaluate the optic pathway or small strokes [1][2][3][6].
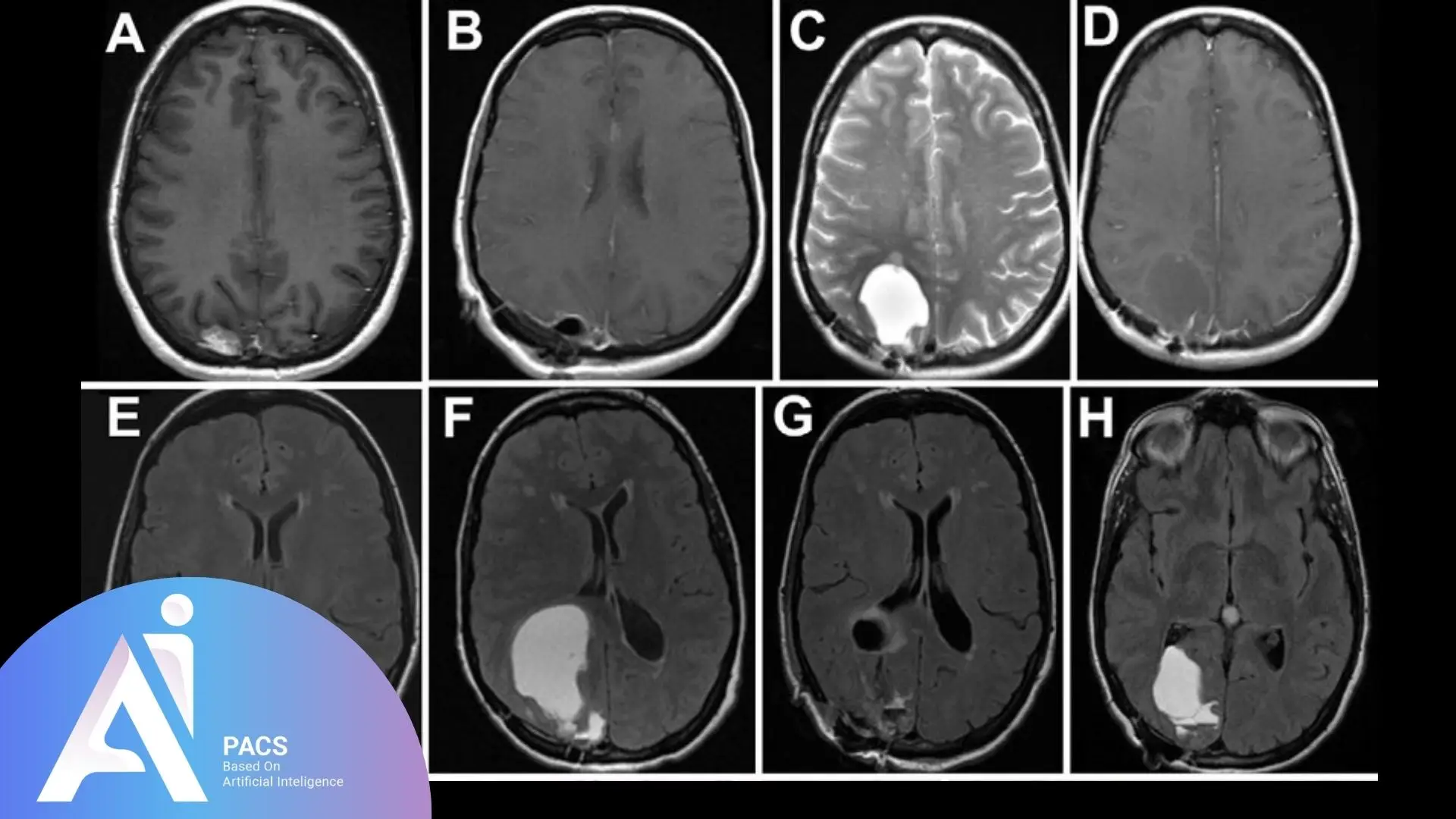
MRI of brain and orbits: what it shows
An MRI protocol for vision problems often includes thin slices through the orbits and brain, with fat suppression and contrast sequences. It can reveal optic neuritis, compressive tumors such as meningioma or pituitary macroadenoma, demyelinating plaques from MS, ischemic injury to the occipital lobes, and posterior reversible encephalopathy syndrome. Diffusion‑weighted imaging can detect early ischemic stroke within minutes to hours [1][2][4][6].
Vessel imaging when blood flow is the concern
If symptoms suggest a stroke or transient ischemic attack, vessel studies may be added. MR angiography or CT angiography can look for carotid or intracranial narrowing, dissection, or aneurysm. Carotid ultrasound may be used when neck vessel disease is suspected. The choice depends on local expertise and how urgent the situation is [1][6].
When is contrast used and is it safe?
Contrast agents make inflammation, tumors, and active lesions light up so they are easier to see. Gadolinium is the MRI contrast. Iodine-based contrast is used for CT angiography and some CT scans. Most patients tolerate contrast well. Your team will check kidney function, allergies, and specific risks before use. Contrast is chosen only when it is likely to change management [2][5].
Common mimics and limits
Migraine aura can cause visual zigzags or blind spots and may have a normal MRI. Functional vision loss and dry eye can mimic neurologic disease. Early CT can miss small occipital strokes, and early optic neuritis may be subtle on imaging, so clinical exam remains essential. Imaging complements, not replaces, a skilled eye and neurologic assessment [1][3][4].
Where PET fits
PET is rarely needed for routine visual symptoms. It may be considered in select cases to evaluate suspected cancer spread or inflammation that remains unclear after MRI and CT [1].
What The Report Means & Next Steps
Your report will describe the area imaged, key findings, and an impression. Look for clear answers to three questions: where is the problem, what is it most likely to be, and what to do next. Reports often recommend correlation with eye exam, blood tests, or follow‑up imaging. Bring the report to your clinician. Ask about any urgent items, what might have been missed, and timelines for follow‑up or treatment changes.
Final Thoughts
Vision changes should never be ignored. Medical imaging helps find the cause, which may be the eye, nerve, or brain.
With the proper scan at the right time, doctors can start treatment early and prevent vision loss. This underscores the importance of not delaying medical imaging. And if you’re unsure what to do, AI-PACS is here to help.
References
- American College of Radiology. ACR Appropriateness Criteria: Orbits, Vision and Visual Loss. https://acsearch.acr.org/list?topic=Orbits,%20Vision%20and%20Visual%20Loss
- org. MRI of the Head. https://www.radiologyinfo.org/en/info/headmr
- org. CT of the Head. https://www.radiologyinfo.org/en/info/cthead
- National Eye Institute. Optic neuritis. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/optic-neuritis
- org. Contrast Materials. https://www.radiologyinfo.org/en/info/safety-contrast
- AHA/ASA. 2019 Update to the 2018 Guidelines for Early Management of Acute Ischemic Stroke. https://www.ahajournals.org/doi/10.1161/STR.0000000000000211
Disclaimer: This article is educational and not a substitute for medical care.